Kidney infection is a type of upper urinary tract infection that reaches the renal tissue, commonly called pyelonephritis. It often starts as a lower‑tract problem like cystitis, a bladder inflammation caused by bacteria, usually Escherichia coli. Understanding the link between these two conditions helps you catch trouble early, avoid hospital stays, and protect kidney health.
From the Bladder to the Kidneys: How an Infection Spreads
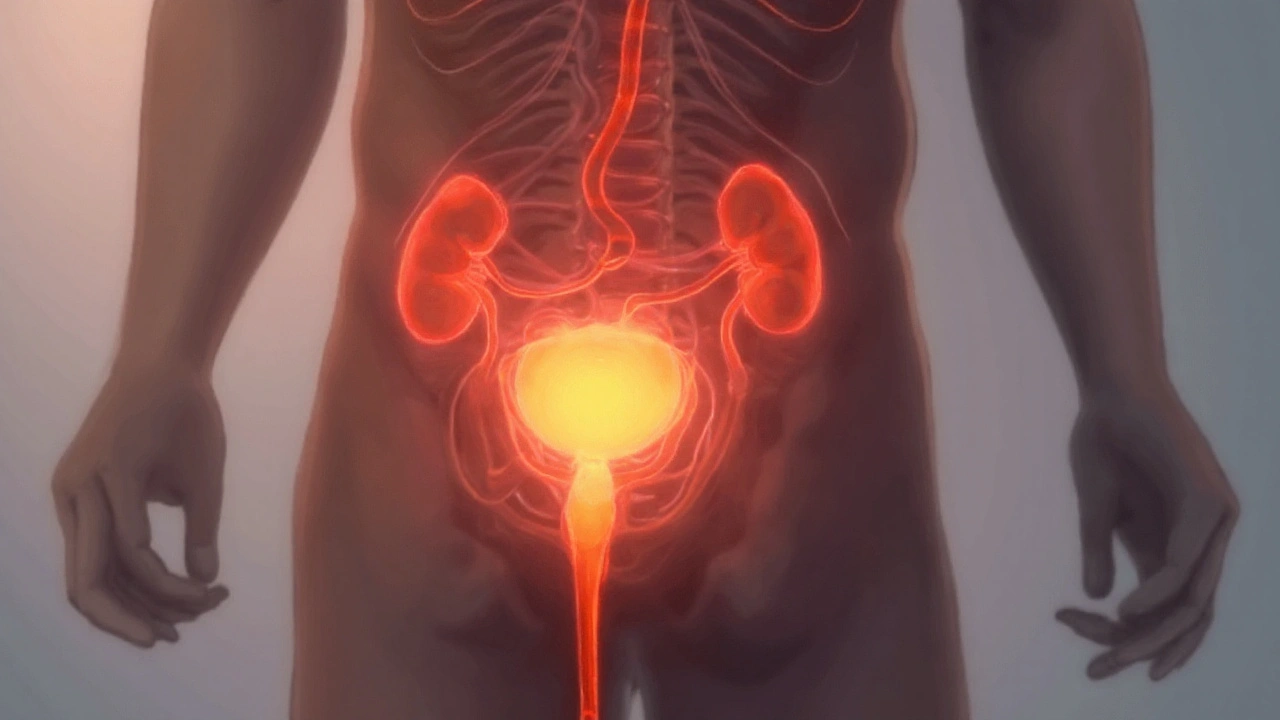
The urinary system is a one‑way pipeline: kidneys filter blood, produce urine, which flows down ureters into the bladder, then out through the urethra. When bacteria colonise the bladder, they sit in a warm, moist environment - perfect for rapid growth. If the immune system or treatment doesn’t clear the microbes, they can travel up the ureters, breach the renal capsule, and inflame the kidney tissue.
What Is Cystitis?
Cystitis is a lower‑tract urinary infection that inflames the bladder lining. About 70% of cases are caused by Escherichia coli, a gut bacterium that migrates to the urethra during sexual activity, poor hygiene, or after catheterisation.
- Typical symptoms: burning during urination, urgency, cloudy or foul‑smelling urine, and mild lower‑abdominal pain.
- Risk factors: frequent sexual intercourse, inadequate hydration, diabetes, and anatomical anomalies like vesicoureteral reflux (urine flowing back toward the kidneys).
Most uncomplicated cystitis resolves with a short course of antibiotics such as trimethoprim‑sulfamethoxazole or nitrofurantoin. However, delayed treatment or resistant bacteria raise the odds of upward spread.
Kidney Infection (Pyelonephritis) Explained
Pyelonephritis is a renal infection that can cause fever, flank pain, and systemic illness. Unlike cystitis, it often produces high‑grade fever, chills, and nausea because the infection breaches the kidney’s vascular network.
- Severity ranges from mild, outpatient‑treated cases to severe sepsis requiring IV antibiotics and hospitalisation.
- Complications include renal abscess, scarring, and chronic kidney disease if infections recur.
Because the kidney is a highly vascular organ, bacteria entering the bloodstream from a urinary source can trigger systemic inflammation, a scenario doctors treat aggressively.
Why Cystitis Turns Into Pyelonephritis
Three main mechanisms push a bladder infection upward:
- Ascending migration: Bacteria travel up the ureters, especially when ureteral peristalsis is impaired or reflux is present.
- Delayed or ineffective treatment: Incomplete antibiotic courses or resistant strains leave residual bacteria that continue proliferating.
- Host vulnerability: Conditions like diabetes, pregnancy, or immunosuppression reduce the body’s ability to clear infection quickly.
Studies from New Zealand hospitals (2023) show that 12% of women presenting with uncomplicated cystitis develop pyelonephritis within two weeks if they skip antibiotics.
Key Risk Factors & Prevention Strategies
Understanding the drivers helps you lower your odds:
- Hydration: Drinking at least 2L of water daily dilutes urine, flushing bacteria out before they can cling to the bladder wall.
- Proper hygiene: Wiping front‑to‑back and urinating after sex cut down bacterial transfer.
- Control of chronic diseases: Keeping blood glucose under 7mmol/L reduces sugar in urine, a food source for bacteria.
- Avoid prolonged catheter use: Catheters bypass natural defenses; if needed, replace them every 7‑10 days.
- Screen for reflux: Children and recurrent adult cases benefit from imaging to detect vesicoureteral reflux.
Diagnosis: From Urine Sample to Imaging
A definitive diagnosis hinges on a urine culture. The lab reports bacterial count (≥10⁵CFU/mL) and antibiotic sensitivity, guiding targeted therapy.
If pyelonephritis is suspected, doctors may order an ultrasound or CT scan to look for swelling, abscesses, or obstruction. Blood tests (elevated CRP, leukocytosis) support systemic involvement.
Treatment Pathways
Both conditions require antibiotics, but the regimen differs:
- Cystitis: Oral antibiotics for 3‑5days; common choices include nitrofurantoin (100mg BID) or fosfomycin (single 3g dose).
- Kidney infection: Oral fluoroquinolones (e.g., ciprofloxacin 500mg BID) for 10‑14days, or IV antibiotics (ceftriaxone) for severe cases.
Patients must finish the full course, even if symptoms improve, to prevent relapse and resistance.
| Feature | Cystitis (Bladder) | Kidney Infection (Pyelonephritis) |
|---|---|---|
| Primary location | Bladder wall | Renal parenchyma |
| Common symptoms | Burning urination, urgency | Fever, flank pain, nausea |
| Typical bacteria | E. coli | E. coli (often resistant strains) |
| Treatment duration | 3‑5days oral | 10‑14days oral or IV |
| Risk of complications | Low (if treated) | High - possible abscess, sepsis |
Related Concepts to Explore
Once you grasp the cystitis‑pyelonephritis link, you’ll encounter these adjacent topics:
- Sepsis: A systemic response that can emerge from an untreated kidney infection.
- Chronic kidney disease: Repeated infections may scar renal tissue, reducing function over time.
- Antibiotic resistance: Overuse of broad‑spectrum drugs fuels resistant E. coli strains.
Future posts will dive deeper into each of these, helping you stay ahead of potential health pitfalls.
What to Do If You Suspect an Infection
- Increase fluid intake - aim for clear, pale urine.
- Monitor symptoms: burning, urgency, fever, flank pain.
- Visit a GP promptly; request a urine culture if symptoms persist beyond 24hours.
- Follow the prescribed antibiotic regimen exactly.
- Seek emergency care if you develop high fever, chills, or vomiting - these may signal pyelonephritis.
Early action cuts the chance of a simple bladder infection turning into a serious kidney problem.
Frequently Asked Questions
Can cystitis resolve on its own without antibiotics?
Mild cases sometimes clear with increased hydration and bladder flushing, but relying on self‑resolution risks bacterial ascent. Health guidelines recommend a short course of antibiotics to guarantee eradication.
What signs tell me that my cystitis has become a kidney infection?
Key red flags include fever >38°C, chills, flank or back pain, nausea, and cloudy or foul‑smelling urine accompanied by systemic malaise. If any appear, seek medical evaluation immediately.
Are there any home remedies that can prevent cystitis from spreading?
Staying well‑hydrated, urinating after sex, avoiding irritating feminine products, and using cranberry juice (unsweetened) may lower bacterial adhesion. These measures support, but do not replace, medical treatment.
How does diabetes increase the risk of kidney infections?
High blood glucose spills into urine, providing a nutrient‑rich medium for bacteria. Additionally, diabetes impairs immune cell function, making it harder to clear infections that have reached the kidneys.
Is it safe to take over‑the‑counter pain relievers while on antibiotics for a kidney infection?
Paracetamol or ibuprofen can help control fever and pain, but always check with your doctor for drug interactions, especially if you have kidney impairment.

dan koz
September 23, 2025 AT 05:22