Every year, tens of thousands of people in developing nations die not because they lack access to medicine, but because the medicine they take is fake. It doesn’t contain the right ingredients. It might have poison in it. Or it might do nothing at all. And most people have no way to tell the difference.
What Exactly Are Counterfeit Drugs?
Counterfeit drugs aren’t just cheap knockoffs. They’re dangerous frauds. The World Health Organization divides them into two types: substandard and falsified. Substandard medicines are real products that were made poorly-maybe they expired, got stored wrong, or were diluted during transport. Falsified medicines are outright fakes. They’re made to look like the real thing, but they’re produced in secret labs with no oversight. Some have no active ingredient at all. Others have too little. A few even contain toxic chemicals like rat poison or industrial solvents.
In high-income countries, the chance of getting a fake medicine is less than 1%. In some parts of Africa and Southeast Asia, it’s over 30%. In certain border towns, half of all malaria pills are counterfeit. These aren’t rare cases. They’re the norm in places where regulation is weak and poverty is high.
Why This Is a Deadly Problem
The numbers are horrifying. In 2018, the WHO estimated that falsified anti-malarial drugs alone caused more than 116,000 deaths in sub-Saharan Africa each year. A 2020 OECD report linked counterfeit medicines to between 72,000 and 169,000 child deaths from pneumonia annually. These aren’t abstract figures. These are children who didn’t get better because their medicine was empty. Parents who gave their kids pills that made them sicker.
It’s not just about immediate poisoning. The bigger threat is drug resistance. When antibiotics don’t have enough active ingredient, they don’t kill all the bacteria. They just make them stronger. That’s how superbugs form. Dr. Gottfried Hirnschall of the WHO warned that counterfeit drugs are making malaria, tuberculosis, and even common infections harder to treat worldwide.
One of the worst cases happened in Lahore, Pakistan, in 2012. Over 200 people died after being given heart medication contaminated with a toxic chemical. The drugs had passed through multiple distributors and were sold in public hospitals. No one tested them. No one checked.
How Fake Drugs Get Into the System
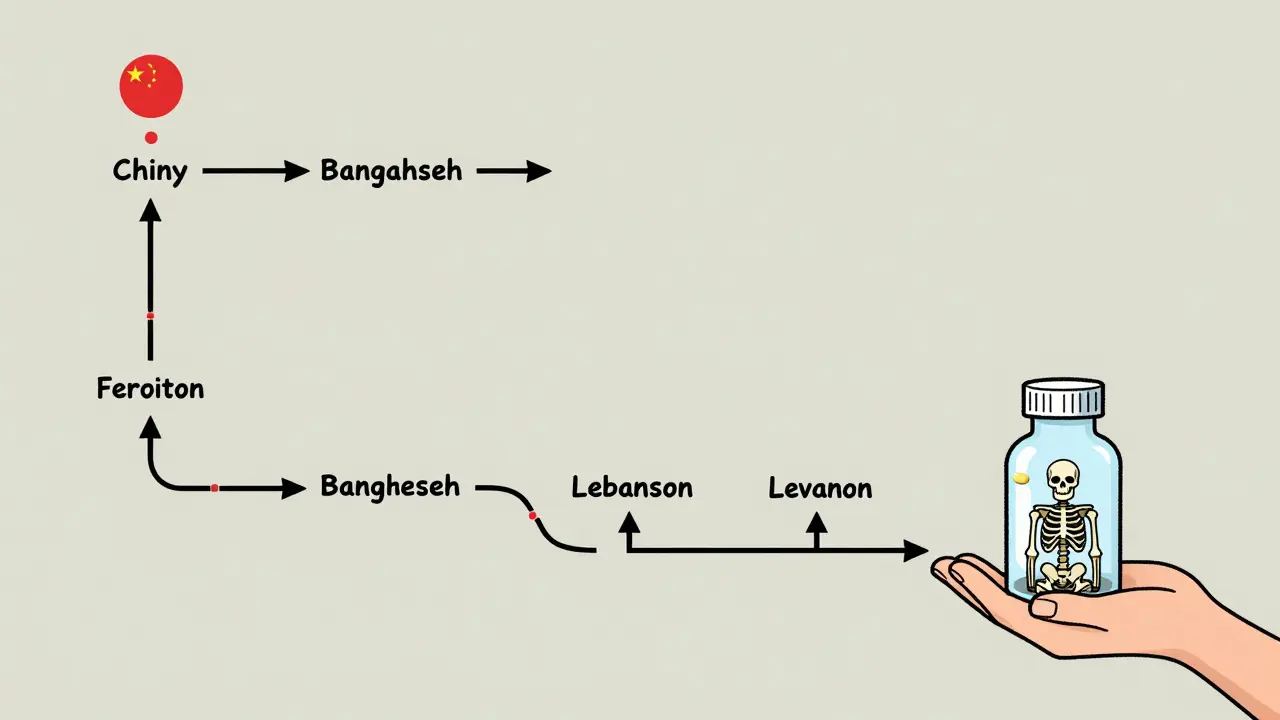
Counterfeit drugs don’t appear out of nowhere. They move through long, messy supply chains. A fake pill might start in a lab in China, then be shipped to Bangladesh, repackaged in Lebanon, smuggled across borders, sold by street vendors, and finally bought by someone who can’t afford the real thing. There can be five to seven middlemen between the factory and the patient. Each stop is a chance for the product to be swapped, diluted, or tampered with.
China produces about 78% of the most convincing fake medicines-packaging that looks identical to the real thing, down to the font and color. But other countries are catching up. Bangladesh, Lebanon, Syria, and Turkey are now major hubs for regional distribution. Criminal networks use 3D printing to replicate blister packs with 99% accuracy. They even copy security features like holograms and QR codes.
Online pharmacies make it worse. In Southeast Asia, 68% of negative reviews on pharmacy websites mention fake pills. People report pills that dissolve too fast, don’t work at all, or cause vomiting and dizziness. Many buyers don’t realize they’re buying from scammers-they think they’re just getting a discount.
Why People Buy Them
It’s not stupidity. It’s survival.
In many developing countries, a real course of malaria treatment can cost three to five times more than a fake one. For families living on less than $2 a day, that’s the difference between buying medicine and buying food. Even if they suspect the pills are fake, they take them anyway-because doing nothing means certain death.
There’s also a lack of trust in the system. In Nigeria, a Reddit user shared that their brother died of malaria after taking counterfeit Coartem. The pharmacy had no way to verify authenticity. In Kenya, healthcare workers found that half the malaria test kits in rural clinics were fake. When you can’t trust your own health system, you’re forced to take risks.
How to Spot a Fake Medicine (And Why It’s Almost Impossible)
Most people think they can tell a fake by looking at the packaging. They’re wrong.
Counterfeiters copy labels, batch numbers, and even expiration dates with 90% accuracy. The pills might look, smell, and taste the same. The only way to be sure is through lab testing-spectroscopy or chemical analysis. But those machines cost tens of thousands of dollars. In rural clinics across sub-Saharan Africa, 85% don’t have access to them.
Simple test kits exist-they cost $5 to $10 and give 70% accuracy. But they require training. In many places, healthcare workers haven’t been trained to use them. Electricity is unreliable. The kits expire. The manuals are in English, not local languages.
Some countries are trying new solutions. Ghana uses a system called mPedigree, where you text a code from the pill pack to a number and get a reply saying if it’s real. One user in Ghana said it saved her child’s life. But only 28% of people in low-literacy areas can use it without help. And not every medicine has the code.

What’s Being Done
There are glimmers of hope.
In 2025, the WHO launched the Global Digital Health Verification Platform, using blockchain to track every pill from manufacturer to patient. So far, it’s active in 27 countries. Pfizer has prevented over 302 million counterfeit doses from reaching patients since 2004 using its own tracking system.
Interpol’s 2025 Operation Pangea XVI shut down 13,000 websites, arrested 769 people, and seized 50 million fake doses. The Medicrime Convention, signed by 76 countries, is the first international treaty to treat counterfeit medicine as a crime-not just a trade issue.
Some solutions are low-tech and local. Solar-powered verification devices now work in 12 African countries. Community health workers are being trained to spot fake packaging and report suspicious pharmacies. In pilot areas, these programs cut counterfeit use by 37%.
The EU is pledging €250 million by 2026 to strengthen medicine safety in 30 developing nations. The WHO aims to reduce counterfeit drug prevalence to under 5% by 2027.
What Needs to Happen Next
Technology alone won’t fix this. The real problem is systemic.
First, governments need to enforce laws. In many countries, selling fake medicine carries the same penalty as selling counterfeit handbags. That’s not enough. Criminals make 9,000% profit on these drugs. The punishment should match the damage.
Second, real medicines need to be affordable. If people can’t buy the real thing, they’ll buy the fake one. Generic drug programs must be expanded and subsidized. Price controls aren’t just ethical-they’re lifesaving.
Third, we need to empower local communities. Training nurses, pharmacists, and even shopkeepers to recognize and report fakes is more effective than any high-tech system. When people know what to look for, they become part of the solution.
And finally, global supply chains must be made transparent. Right now, a fake drug can cross five borders before anyone checks it. We need real-time tracking, shared databases, and joint inspections between countries.
The Bottom Line
Counterfeit drugs aren’t just a health issue. They’re a justice issue. People in poor countries aren’t getting second-rate medicine-they’re getting no medicine at all. And they’re dying for it.
Every fake pill sold is a betrayal. A betrayal of trust. A betrayal of science. A betrayal of human life.
The tools to stop this exist. The knowledge exists. What’s missing is the will. Until governments, drug companies, and global health organizations treat this crisis with the urgency it deserves, more people will keep dying-quietly, invisibly, and needlessly.
Kegan Powell
January 28, 2026 AT 07:49