Antibiotic Liver Injury Risk Calculator
Calculate Your Risk
This tool estimates the type and risk level of antibiotic-induced liver injury based on clinical parameters from the article.
Antibiotics save lives. But for some people, the very drugs meant to fight infection can quietly damage the liver - sometimes without warning. This isn’t rare. In fact, antibiotics cause about 64% of all drug-induced liver injury cases, especially in hospitalized patients. The damage often shows up as either hepatitis (liver cell inflammation) or cholestasis (blocked bile flow), and it’s easy to miss because symptoms can be vague or masked by the original illness.
How Antibiotics Hurt the Liver
It’s not just one way antibiotics cause liver injury. They attack from multiple angles. Some interfere with mitochondria - the energy factories inside liver cells. When these get damaged, cells start to die. Others turn into toxic chemicals inside the liver, poisoning nearby tissue. And then there’s the gut. Antibiotics wipe out good bacteria, letting harmful ones take over. This breaks down the gut barrier, letting toxins leak into the bloodstream and reach the liver.
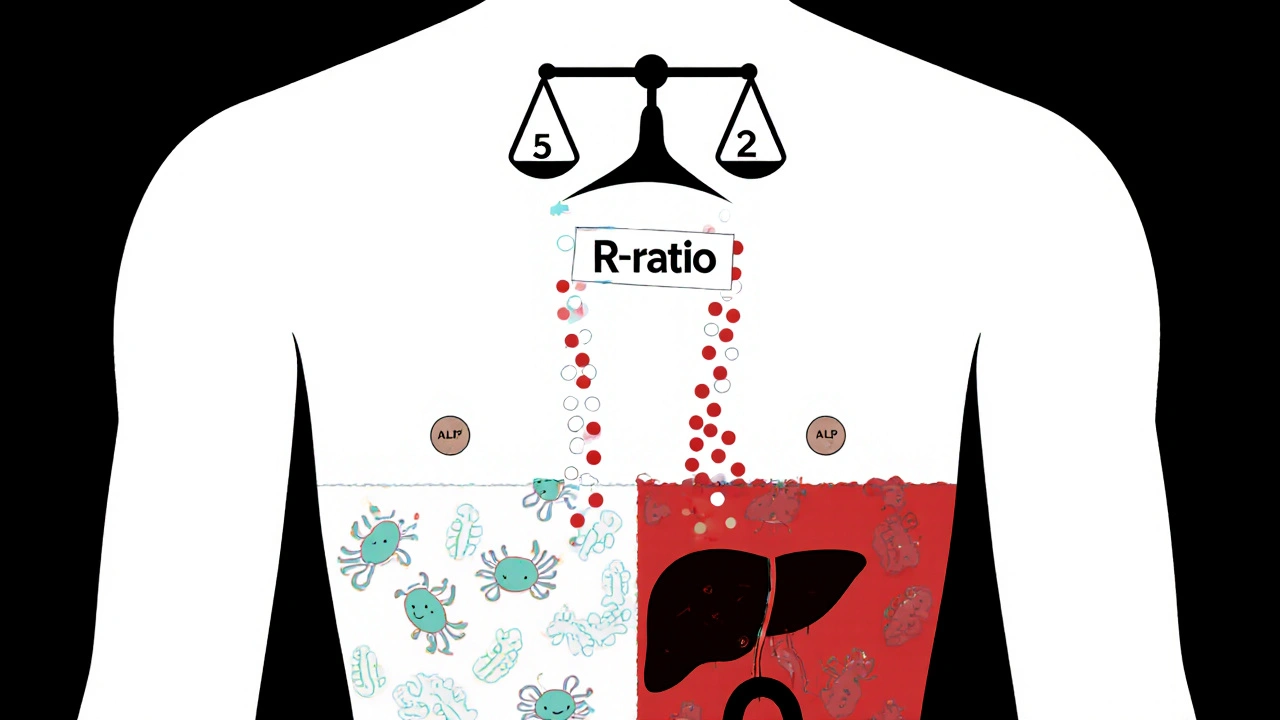
These mechanisms explain why two main patterns show up in blood tests: hepatocellular injury and cholestatic injury. Hepatocellular means liver cells are dying - ALT levels spike above 5 times the normal limit. Cholestatic means bile isn’t flowing - ALP levels climb above 2 times normal. Sometimes, you get both. Doctors use something called the R-ratio to tell them which pattern they’re seeing: R > 5 = hepatocellular, R < 2 = cholestatic, and anything in between is mixed.
Which Antibiotics Are the Worst?
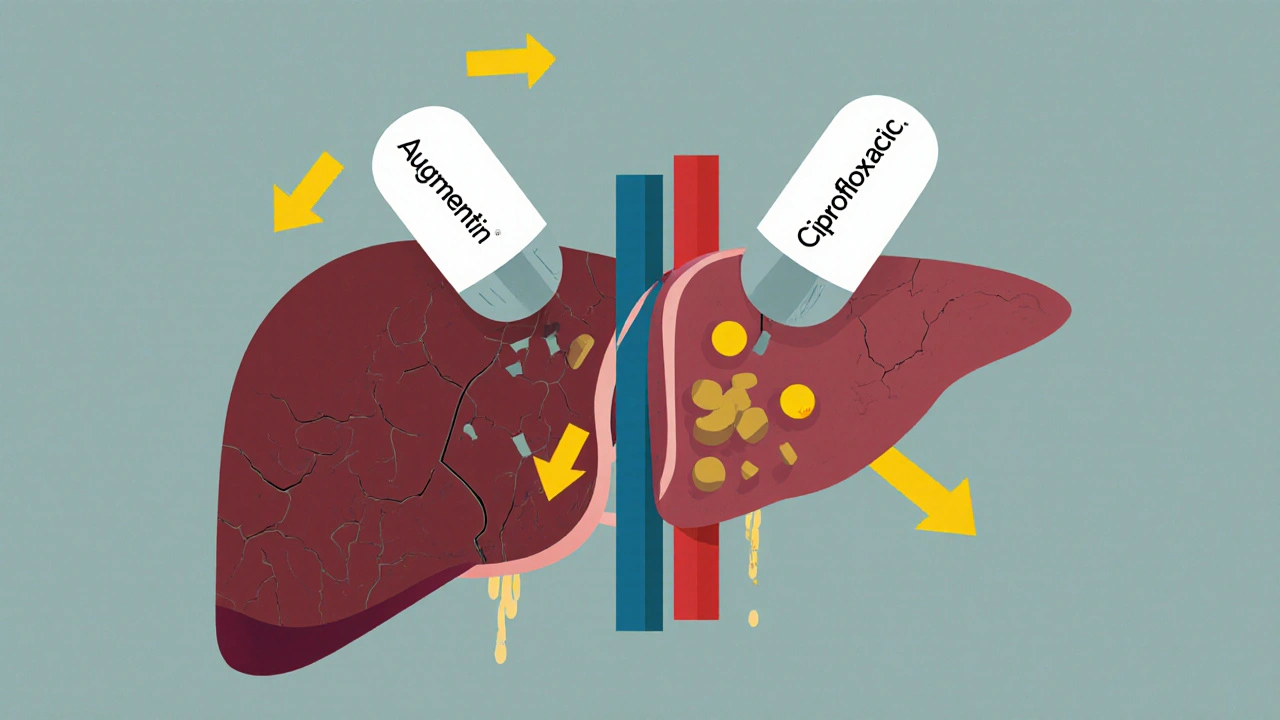
Not all antibiotics carry the same risk. Some are far more likely to cause trouble. Amoxicillin-clavulanate (Augmentin) tops the list. About 15 to 20 people out of every 100,000 who take it will develop liver injury. Most of those cases are cholestatic - meaning bile flow slows or stops. The injury usually shows up 1 to 6 weeks after starting the drug.
Fluoroquinolones like ciprofloxacin and azithromycin are less common culprits, but they often cause mixed injury. They can hit liver cells and bile ducts at the same time. In ICU patients, piperacillin-tazobactam (TZP) is especially dangerous. One study found nearly 29% of patients on TZP for more than 7 days developed liver injury - more than double the rate seen with meropenem. And men are 2.4 times more likely than women to get liver damage from meropenem.
Even older drugs like rifampin and isoniazid - often used for tuberculosis - can be risky, especially when taken together. Isoniazid alone isn’t a major problem, but combined with rifampin, the liver gets hit harder. Nitrofurantoin and trimethoprim-sulfamethoxazole are moderate-risk, but still worth watching, especially in older adults or people with kidney problems.
When Does It Happen?
Timing matters. The longer you’re on antibiotics, the higher your risk. If you take them for 7 days or more, your chance of liver injury jumps by more than 3 times. That’s why doctors are now pushing back on long courses for simple infections like sinusitis or bronchitis - where antibiotics often aren’t even needed.
Onset varies by drug. Augmentin? Usually 2 to 4 weeks in. Ciprofloxacin? Sometimes as early as 5 to 10 days. In ICU patients, where multiple antibiotics are used and patients are already sick, liver injury can sneak up fast. Sometimes, it’s only caught because routine blood tests show ALT or ALP climbing - even if the patient feels fine.
Who’s at Risk?
It’s not just about the drug. The person matters too. People with sepsis are 1.8 times more likely to develop antibiotic-related liver injury. Older adults, those with existing liver disease, and people on multiple medications are also at higher risk. Genetics play a role too. Some people carry specific HLA gene variants that make them more sensitive to certain antibiotics. That’s why two people taking the same drug at the same dose can have totally different outcomes - one is fine, the other ends up in the hospital.
And here’s the kicker: you can’t always predict who will react. That’s why it’s called idiosyncratic - it’s unpredictable. But we’re getting better at spotting the signs early.
How Doctors Spot It
There’s no single test for antibiotic-induced liver injury. Diagnosis is mostly a process of elimination. First, they check the timing - did the liver enzymes rise after starting the antibiotic? Second, they rule out other causes: viral hepatitis, alcohol, fatty liver, gallstones, or even heart failure. In the ICU, that’s hard. Patients often have septic shock, low blood pressure, or multiple organ failures - all of which can raise liver enzymes.
Doctors rely on lab values. ALT > 5× ULN? That’s a red flag for hepatitis. ALP > 2× ULN? That points to cholestasis. If bilirubin is also above 2× ULN, it’s a sign of serious damage. Many hospitals follow the “rule of 5”: stop the antibiotic if ALT is more than 5 times normal, or if ALP is more than 2 times normal and the patient has symptoms like jaundice, nausea, or dark urine.
The LiverTox database from the National Institutes of Health is a go-to resource. It rates antibiotics on a 10-point scale. Augmentin? Score of 9 - high risk. Ciprofloxacin? Score of 6 - moderate. It’s updated regularly and used by clinicians worldwide.

What Happens After Stopping the Drug?
Good news: in most cases, the liver heals itself. Once the antibiotic is stopped, enzymes usually start dropping within days. Jaundice fades. Energy returns. Full recovery happens in 80% of patients within 3 months.
But not everyone recovers. About 5% develop severe liver failure and need a transplant. A small number - less than 1% - die. That’s why catching it early is critical. Delayed diagnosis can turn a reversible injury into something life-threatening.
How to Prevent It
Prevention starts with smart prescribing. Don’t give antibiotics unless they’re truly needed. For infections like earaches or sore throats, watchful waiting often works better than rushing to a pill.
When antibiotics are necessary, monitor. Baseline liver tests before starting are recommended - especially for high-risk drugs. Follow-up tests at 1 to 2 weeks for drugs like Augmentin. For ICU patients on long courses, weekly checks are standard. If enzymes start rising, don’t wait. Re-evaluate the antibiotic. Is there a safer alternative? Can the dose be lowered? Can the course be shortened?
Emerging tools might help soon. Researchers are testing gut microbiome tests to predict who’s at risk. One study found people with low levels of Faecalibacterium prausnitzii - a good gut bacterium - had 3.7 times higher risk of liver injury. Probiotics are being tested in clinical trials to see if they can protect the liver during antibiotic treatment. Results are expected in 2025.
The Bigger Picture
This isn’t just a medical problem - it’s a financial one. Antibiotic-related liver injury costs the U.S. healthcare system over $768 million a year. Drug companies avoid developing new antibiotics because liver toxicity kills 19% of candidates before they even reach patients.
Regulators like the FDA and EMA now require stricter monitoring for new antibiotics. But the real change will come from personalized medicine. In the next 5 to 7 years, genetic testing may tell doctors which antibiotics are safe for you - based on your HLA profile. That could cut liver injury rates by 30 to 40%.
For now, awareness is the best tool. If you’re on antibiotics and start feeling unusually tired, notice yellowing of your skin or eyes, or have dark urine and pale stools - speak up. Your liver might be sending a signal.
Can antibiotics cause liver damage even if I feel fine?
Yes. Many people with antibiotic-related liver injury have no symptoms at first. The first sign is often abnormal blood tests - elevated ALT or ALP - found during routine monitoring. That’s why doctors recommend checking liver function before and during treatment with high-risk antibiotics, especially if you’re on them for more than a week.
Is liver damage from antibiotics permanent?
In most cases, no. Once the antibiotic is stopped, the liver usually repairs itself over weeks to months. About 80% of patients fully recover. But in rare cases - less than 5% - the damage can be severe enough to cause liver failure, requiring a transplant. Early detection and stopping the drug quickly are the best ways to prevent lasting harm.
Which antibiotic is most likely to cause liver injury?
Amoxicillin-clavulanate (Augmentin) carries the highest risk among commonly used antibiotics. About 15 to 20 cases of liver injury occur per 100,000 prescriptions. It most often causes cholestatic injury, meaning bile flow slows down. The injury typically appears 1 to 6 weeks after starting the drug.
How long should I be monitored for liver damage while on antibiotics?
For high-risk antibiotics like amoxicillin-clavulanate, baseline liver tests should be done before starting, and a repeat test after 1 to 2 weeks. For patients on long courses (7+ days), especially in the ICU, weekly monitoring is recommended. If liver enzymes start rising, doctors may stop the drug early - even before symptoms appear.
Can probiotics help prevent antibiotic-related liver injury?
Early research suggests yes. Antibiotics disrupt gut bacteria, which can trigger liver inflammation. Clinical trials are testing whether specific probiotics can restore gut balance and lower liver injury risk. Two major trials are underway, with results expected in 2025. While not yet standard practice, some doctors recommend probiotics for patients on long-term antibiotics, especially if they’ve had liver issues before.
Manuel Gonzalez
November 1, 2025 AT 06:03