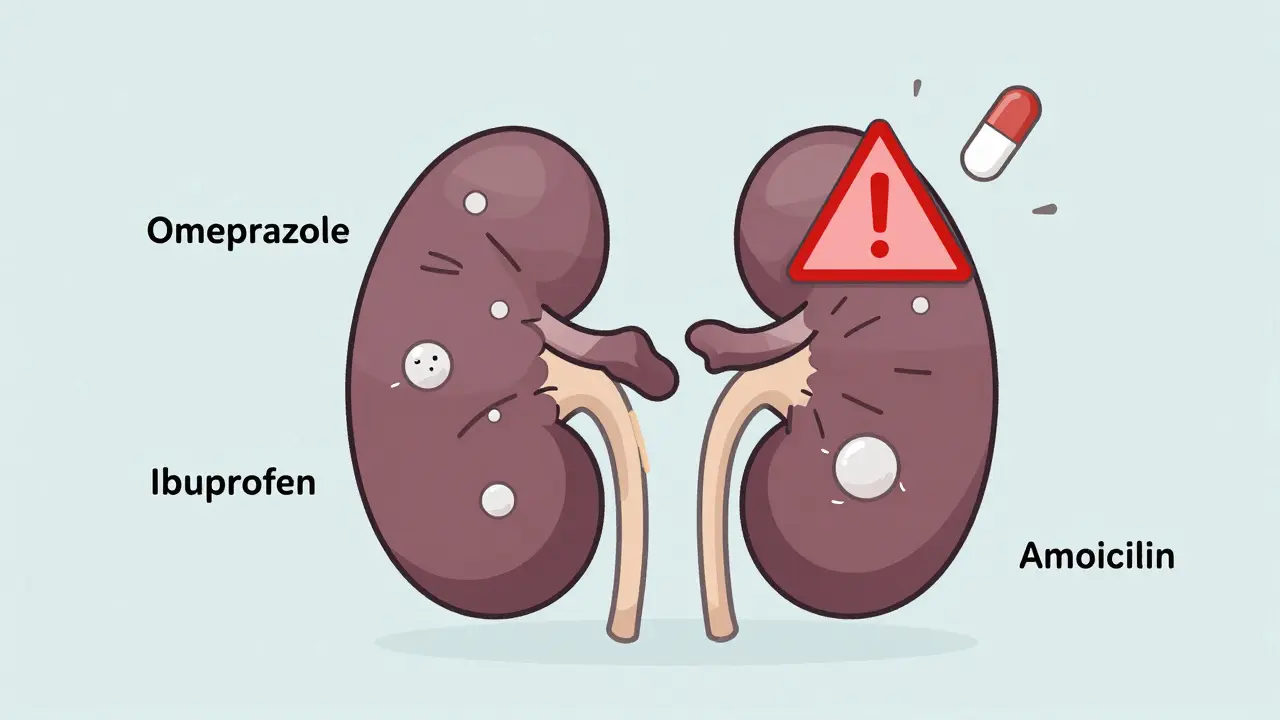
When your kidneys start acting up-swelling, fatigue, little urine output-it’s easy to blame a cold, a UTI, or just dehydration. But if you’ve been taking common medications like omeprazole, ibuprofen, or amoxicillin for weeks or months, you might be dealing with something more serious: acute interstitial nephritis (AIN). It’s not rare. In fact, drugs cause 60-70% of all cases. And most people have no idea until their kidney function drops sharply.
What Actually Happens in Your Kidneys?
Your kidneys don’t just filter waste. They regulate blood pressure, balance electrolytes, and make red blood cells. The tiny spaces between the kidney tubules-called the interstitium-are where inflammation strikes in AIN. It’s not a blockage. It’s an immune reaction. Your body mistakes a drug for a threat and sends in white blood cells, eosinophils, and other immune fighters. They swarm the area, causing swelling, scarring, and disruption to the filtering process.This isn’t a slow decline. It hits fast. Creatinine levels spike. GFR (glomerular filtration rate) drops. You might not feel sick at first. Some people only notice they’re urinating less, or they’re tired all the time. Others get fever, rash, or joint pain. But here’s the catch: fewer than 10% of cases show the classic “hypersensitivity triad” of rash, fever, and high eosinophils. That means doctors often miss it.
Which Drugs Are the Biggest Culprits?
Over 250 medications have been linked to AIN. But three classes stand out:- Proton Pump Inhibitors (PPIs) - Omeprazole, pantoprazole, esomeprazole. These are everywhere. Used for heartburn, acid reflux, even taken “just in case.” In recent years, PPIs have overtaken antibiotics as the second most common cause. A 2022 global registry found they triggered 38% of AIN cases. The scary part? Even after stopping the drug, only 50-60% of patients fully recover kidney function.
- NSAIDs - Ibuprofen, naproxen, celecoxib. These are taken daily by millions for arthritis or headaches. They cause 44% of drug-induced AIN cases. Unlike other triggers, NSAID-induced AIN often comes with heavy proteinuria (over 3 grams/day), and recovery is slower. People over 50 with existing kidney issues are at highest risk.
- Antibiotics - Penicillins, cephalosporins, sulfonamides, ciprofloxacin. These cause about 33% of cases. They tend to hit fast-symptoms appear in as little as 10 days. You’re more likely to see fever, rash, and eosinophiluria here. But here’s the twist: even though the symptoms are more dramatic, recovery rates are better than with PPIs.
And then there are the newer offenders: immune checkpoint inhibitors used in cancer therapy. These are rare but dangerous. They can trigger AIN that’s hard to reverse, even with steroids.
How Do You Know It’s AIN and Not Something Else?
There’s no blood test that confirms it. Urine tests might show white blood cells, eosinophils, or protein-but they’re not reliable. A 67-gallium scan? Too vague. A kidney biopsy? That’s the gold standard.Doctors won’t jump to biopsy unless they’re sure. But if you’ve had a sudden drop in kidney function, are on one of these drugs, and have no other clear cause (like dehydration or sepsis), a biopsy becomes urgent. Waiting too long means the inflammation turns to fibrosis-permanent scarring. That’s when your kidney function doesn’t bounce back.
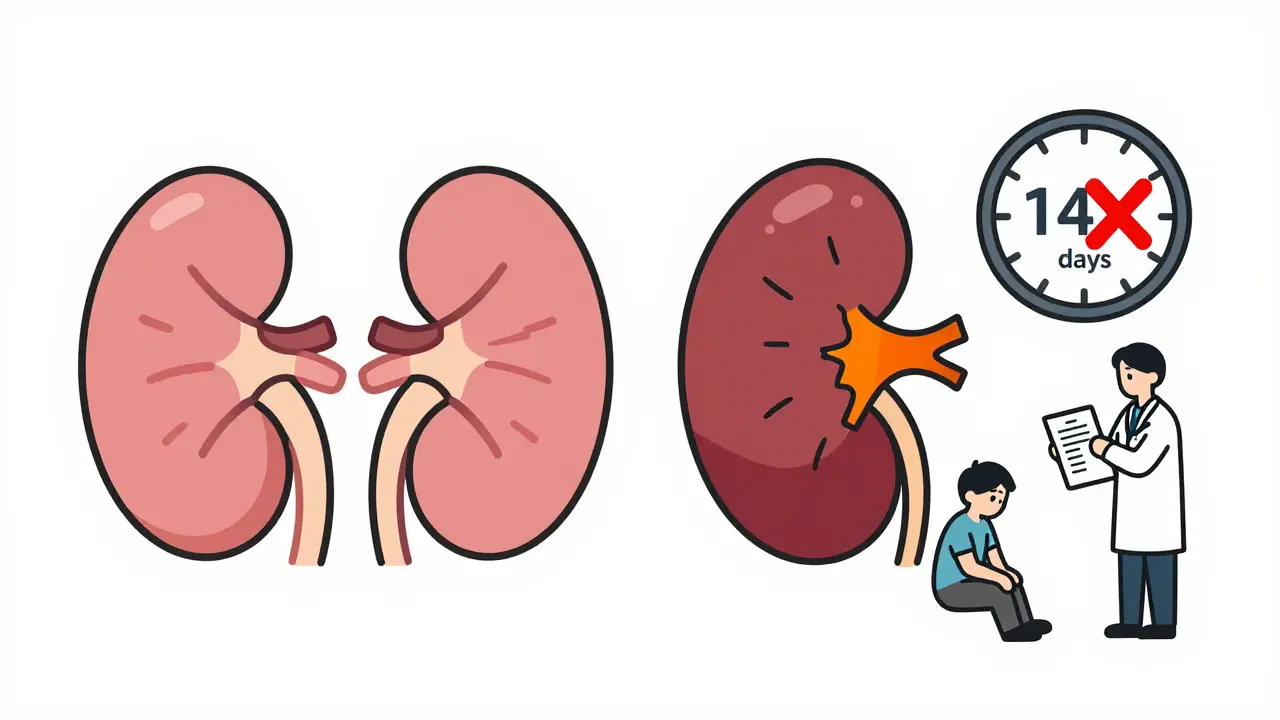
One study found that patients diagnosed within 7 days had a 35% higher chance of full recovery than those diagnosed after 14 days. That’s the window. Two weeks. That’s all you get.
Recovery Isn’t Guaranteed-Even After Stopping the Drug
Stopping the drug is step one. And it’s critical. In 65% of cases, people start feeling better within 72 hours of quitting the medication. But “feeling better” doesn’t mean “fixed.”Recovery timelines vary:
- Antibiotic-induced: median 14 days
- NSAID-induced: median 28 days
- PPI-induced: median 35 days
And here’s what patients don’t talk about enough: 42% of those surveyed still had eGFR under 60 mL/min/1.73m² six months later. That’s stage 3 chronic kidney disease. For NSAID users, the risk of long-term damage jumps to 42%. PPI users? Around 30-35%. Even if you stop the drug, the damage might stick.
A case from the American Kidney Fund tells the story: a 63-year-old woman took omeprazole for 18 months. She developed AIN. She needed dialysis for three weeks. Her eGFR improved-but stayed at 45. She’s now in permanent stage 3 kidney disease.
Do Steroids Help? The Controversy
There’s no large randomized trial proving corticosteroids work. But in real-world practice, doctors use them. Why? Because when kidney function is crashing-eGFR under 30-or if it keeps dropping after stopping the drug, steroids can make the difference.The protocol? Start with methylprednisolone (0.5-1 mg/kg/day) for 2-4 weeks, then switch to oral prednisone and taper slowly over 6-8 weeks. The European Renal Association says this is the most common approach. But it’s not without risk. Weight gain, mood swings, blood sugar spikes-all real side effects.
Dr. Ronald J. Falk from UNC Kidney Center says it plainly: “Benefits aren’t proven in trials, but when the kidney is failing, we can’t wait for perfect evidence.”
Who’s Most at Risk?
It’s not just about what you take-it’s who you are.- Age 65+: Risk jumps from 5 cases per 100,000 in young adults to 22 per 100,000 in seniors.
- Taking 5+ medications: That multiplies your risk 3.2 times. Polypharmacy is a silent killer for kidneys.
- Pre-existing kidney disease: Even mild CKD makes you far more vulnerable.
- Long-term PPI use: More than 3 months? You’re in the danger zone.
The rise in AIN cases? It’s tied directly to how often we take these drugs. Between 2010 and 2020, drug-induced AIN rose by 27%. PPIs alone now cause 12 cases per 100,000 people every year. That’s not rare. That’s epidemic-level.
What Should You Do?
If you’re on any of these drugs and notice:- Sudden decrease in urine output
- Unexplained fatigue or nausea
- Swelling in legs or face
- Unusual fever or rash
Get your kidney function checked-now. Ask for serum creatinine and eGFR. Don’t wait for “it’ll pass.”
And if you’ve been on PPIs for more than a year? Talk to your doctor about whether you still need them. Many people take them out of habit, not necessity. Same with NSAIDs. Daily ibuprofen? That’s not harmless.
Early detection saves kidneys. Delayed diagnosis? It leads to permanent damage.
What’s Next for AIN?
Researchers are hunting for biomarkers. One promising test looks at urinary CD163-a protein released by immune cells in the kidney. In a 2022 study, it caught 89% of AIN cases without needing a biopsy. If this becomes routine, we could diagnose AIN before kidney damage even happens.But until then? The best defense is awareness. Know your drugs. Know your numbers. And if your kidneys are acting strange? Don’t ignore it.
Can acute interstitial nephritis be reversed?
Yes-but only if caught early. Stopping the drug that caused it can lead to full recovery in 70-80% of antibiotic-induced cases. But with NSAIDs or PPIs, recovery is slower and less complete. About 30-42% of patients end up with permanent kidney damage, especially if diagnosis is delayed beyond two weeks.
How long does it take to recover from drug-induced AIN?
Recovery time depends on the drug. Antibiotics: around 14 days. NSAIDs: about 28 days. PPIs: up to 35 days. Some people start feeling better within 72 hours of stopping the drug, but full kidney function recovery can take weeks or months. In severe cases, dialysis may be needed for 2-6 weeks.
Are proton pump inhibitors (PPIs) really dangerous for kidneys?
Yes. PPIs are now the second most common cause of acute interstitial nephritis. While they may cause milder symptoms than antibiotics, they’re far more commonly used-often for years. Studies show only 50-60% of PPI-induced AIN patients fully recover kidney function, and long-term use increases the risk of chronic kidney disease.
Do I need a kidney biopsy to diagnose AIN?
Yes, it’s the only definitive way. Blood and urine tests can suggest AIN, but they can’t confirm it. A biopsy shows the immune cell buildup in the kidney tissue. Doctors avoid it unless other causes are ruled out-but if your kidney function is dropping fast and you’re on a high-risk drug, biopsy is the fastest path to treatment.
Can AIN come back after recovery?
If you restart the same drug, yes-re-exposure almost always causes recurrence. Even if you recover fully, you should avoid the medication that caused it. Some patients develop sensitivity to entire drug classes (e.g., all NSAIDs). Always tell future doctors about your history of AIN.
Is dialysis always needed for AIN?
No. Only about 15-20% of patients need dialysis, usually in severe cases where creatinine is very high or kidney function keeps worsening. Dialysis is temporary-it supports the body while the kidneys heal. Most patients stop dialysis within 2-6 weeks after removing the drug and starting treatment.
Mike Hammer
February 14, 2026 AT 10:58