Heart disease kills more women than all cancers combined. Yet, most women still don’t realize it’s their biggest health threat. In the U.S. alone, about 307,000 women die from heart disease each year - that’s one in five. And it’s not just older women. Women under 55 are seven times more likely than men to be sent home from the ER with a heart attack misdiagnosed as anxiety or indigestion. The result? A 50% higher chance of dying within a year.
Why Women’s Heart Attacks Don’t Look Like the Movies
When you think of a heart attack, you probably picture someone clutching their chest, doubling over, screaming in pain. That’s the Hollywood version. It’s also the male version. For women, it’s rarely that clear. Women are far more likely to have symptoms that feel like something else entirely. Think: exhaustion so deep you can’t make your bed. Jaw pain that comes and goes. Nausea that feels like food poisoning. Shortness of breath while walking to the mailbox. Dizziness that makes you sit down suddenly. According to the National Heart, Lung, and Blood Institute, only about 65% of women experience chest pain during a heart attack - compared to 90% of men. And when women do feel chest discomfort, it’s often described as pressure, tightness, or a squeezing sensation - not the crushing pain men report. That subtle difference is why so many women wait too long to get help. A 2021 study in the Journal of the American Heart Association found that nearly half of women who had heart attacks didn’t have chest pain at all. Instead, they had fatigue, nausea, back pain, or jaw pain. These symptoms can show up days or even weeks before the actual event. That’s not a coincidence. It’s your body trying to tell you something.The Silent Symptoms Women Ignore - and Doctors Overlook
One of the most dangerous myths is that if you don’t have chest pain, you’re fine. That’s not true - especially for women. Unexplained fatigue is the number one red flag. Not just being tired after a long day. We’re talking about fatigue so severe it stops you from doing simple things: carrying groceries, taking a shower, playing with your kids. In one Yale study, 71% of women who had heart attacks reported this kind of fatigue - but only 16% of men did. And most women assume it’s stress, lack of sleep, or aging. Shortness of breath without exertion is another major sign. If you’re winded climbing one flight of stairs now, when you used to run up them without breaking a sweat, that’s not normal. It’s a sign your heart isn’t pumping efficiently. Jaw, neck, or back pain is also common. Women often describe it as a dull ache or pressure that moves around. It doesn’t feel like a pulled muscle. It doesn’t go away with stretching. It lingers. And it’s often worse at night. Nausea, vomiting, or indigestion can be the only symptoms. Many women go to the doctor thinking they have the flu - only to find out their heart is struggling. The Family Heart Foundation found women are 59% more likely than men to mistake heart attack symptoms for stomach issues. And then there’s mental stress. Women are 37% more likely than men to have angina triggered by emotional stress - a breakup, a family crisis, a work deadline. That’s not just ‘being emotional.’ It’s your heart reacting to pressure in a way men’s hearts rarely do.Why Women’s Hearts Are Different - And Why It Matters
It’s not just about symptoms. Women’s hearts are built differently. Most heart attacks in men happen because of a major artery getting blocked by plaque. In women, it’s often something else:- Microvascular disease: Tiny arteries in the heart become inflamed or narrow. This doesn’t show up on a standard angiogram, so doctors often say, ‘Your arteries look fine.’ But your heart is still starving for blood. This affects nearly twice as many women as men.
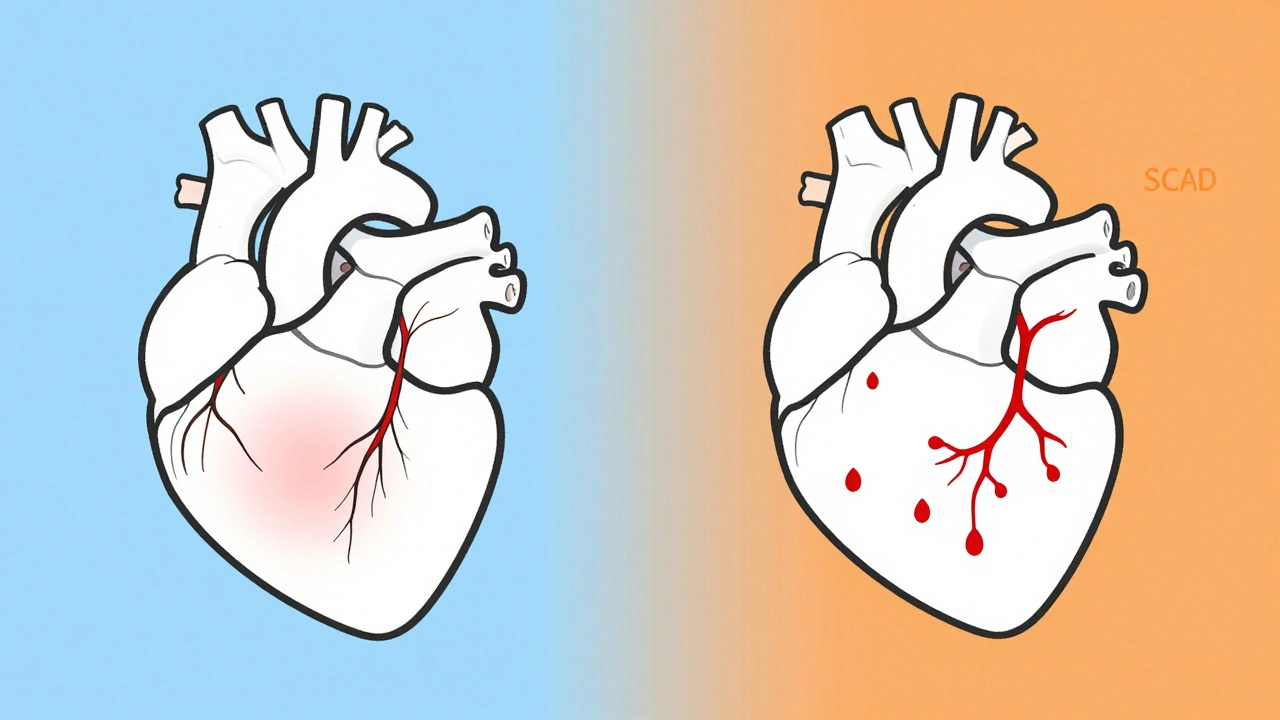
- Spontaneous Coronary Artery Dissection (SCAD): A tear forms in a heart artery - no plaque involved. It’s rare, but it happens mostly in women under 50, often during or after pregnancy. It’s not caused by lifestyle. It can strike healthy, active women with no risk factors.
- Takotsubo syndrome (broken heart syndrome): Extreme emotional stress can temporarily stun the heart, mimicking a heart attack. It’s more common in postmenopausal women.
Hidden Risk Factors Most Women Don’t Know About
You’ve heard about high blood pressure, cholesterol, and smoking. But here are the risks that hit women harder:- Pregnancy complications: If you had preeclampsia, gestational diabetes, or delivered a baby prematurely, your risk of heart disease later in life jumps by 60-80%. This isn’t just ‘something that happened.’ It’s a warning sign.
- Menopause: After menopause, estrogen drops - and so does protection for your arteries. Your LDL (bad cholesterol) rises, your HDL (good cholesterol) falls, and your blood pressure often climbs. That’s why heart disease risk spikes after 50.
- Autoimmune diseases: Lupus, rheumatoid arthritis, and other conditions that cause chronic inflammation increase heart disease risk significantly. Women are far more likely to have these.
- Polycystic ovary syndrome (PCOS): This hormonal disorder is linked to insulin resistance, obesity, and high blood pressure - all major heart disease drivers.
- Silent heart attacks: Women over 65 are 34% more likely than men to have a heart attack with no symptoms at all. They just wake up one day with heart failure - and don’t know why.
What You Can Do - Practical Steps for Prevention and Early Detection
Knowing the risks isn’t enough. You need to act. Track your body. Keep a simple journal: When did you feel unusually tired? Did your jaw ache for no reason? Did you get winded walking to the car? Write it down. Bring it to your doctor. Don’t wait for symptoms to get worse. Ask for the right tests. If you have symptoms but your EKG and blood tests are normal, ask: ‘Could this be microvascular disease?’ or ‘Should I get a coronary CT angiogram?’ Standard stress tests miss up to 70% of microvascular issues in women. Use new tools. The FDA-approved Corus CAD test analyzes gene expression to detect blocked arteries in women with 88% accuracy - far better than traditional tests. Ask your doctor if it’s right for you. Know your numbers: Blood pressure under 120/80. LDL under 100. Fasting blood sugar under 100. HbA1c under 5.7%. If you’re over 40, get these checked yearly. Move - but don’t overdo it. Walking 30 minutes a day cuts heart disease risk by 30%. But if you’re exhausted after a walk, that’s not ‘being out of shape.’ It’s your heart asking for help. Manage stress. Chronic stress raises cortisol, which increases blood pressure and inflammation. Try daily breathing exercises, yoga, or even just 10 minutes of quiet time. Your heart will thank you.
When to Go to the ER - No Excuses
If you have three or more of these symptoms - even if they’re mild - go to the ER:- Unexplained fatigue (lasting more than two weeks)
- Shortness of breath during light activity
- Nausea or vomiting without a clear cause
- Jaw, neck, or back pain
- Lightheadedness or sudden dizziness
Why You Need a Women’s Heart Center
Not all hospitals are created equal. The American College of Cardiology created a certification for Women’s Cardiovascular Centers of Excellence. These centers have protocols specifically designed for women - from faster testing to staff trained to recognize non-chest symptoms. Women treated at these centers are 22% more likely to survive a heart attack. That’s not a small number. That’s life or death. If you’re in the U.S., check if your hospital is certified. If you’re elsewhere, ask your doctor: ‘Do you have experience treating women with heart disease?’ and ‘Have you seen cases of SCAD or microvascular disease?’It’s Not Just About You - It’s About Every Woman Around You
Heart disease doesn’t just affect the woman who has it. It affects her family, her job, her children, her future. And right now, too many women are dying because no one told them what to look for. If you’ve ever said, ‘I’m just tired,’ or ‘It’s probably just stress,’ stop. That’s not normal. That’s your heart speaking. The data is clear. The symptoms are real. The tools exist. What’s missing is awareness - and action. Start today. Talk to your mom, your sister, your best friend. Share this. Ask your doctor for a heart check. Write down your symptoms. Don’t wait for the next heart attack to be the one that doesn’t get a second chance.What are the most common heart attack symptoms in women?
While chest pain can happen, women are more likely to experience unusual fatigue, shortness of breath, nausea, jaw or back pain, dizziness, and cold sweats. Many women don’t have chest pain at all - nearly 43% of female heart attacks occur without it.
Can women have heart attacks without chest pain?
Yes. In fact, nearly half of women who have heart attacks report no chest pain. Symptoms like extreme fatigue, shortness of breath, nausea, or jaw pain can be the only signs. This is why women are often misdiagnosed - their symptoms don’t match the male-dominated textbook image of a heart attack.
What increases a woman’s risk of heart disease beyond the usual factors?
Pregnancy complications like preeclampsia or gestational diabetes increase heart disease risk by up to 80%. Menopause, autoimmune diseases like lupus, PCOS, and chronic stress also raise risk significantly. These are often overlooked in standard risk assessments.
Are standard heart tests accurate for women?
Traditional stress tests and angiograms often miss microvascular disease and SCAD - conditions more common in women. The FDA-approved Corus CAD test, which analyzes gene expression, is 88% accurate in women compared to 72% for standard tests. Ask your doctor if this test is appropriate for you.
Should women go to the ER if they suspect a heart attack but aren’t sure?
Yes. If you have three or more symptoms - such as fatigue, shortness of breath, nausea, jaw/back pain, or dizziness - go to the ER immediately. Waiting even an hour can cause irreversible damage. It’s better to be checked and be fine than to delay and risk death.
What’s the difference between a heart attack and broken heart syndrome?
Broken heart syndrome (Takotsubo cardiomyopathy) is triggered by extreme emotional stress - like grief or shock - and causes temporary heart muscle weakness that mimics a heart attack. It’s more common in postmenopausal women. Unlike a heart attack, there’s usually no artery blockage, and the heart often recovers fully with time and care.
Can lifestyle changes prevent heart disease in women?
Yes - but not always. While healthy eating, exercise, and not smoking help, many women develop heart disease due to factors beyond lifestyle - like pregnancy complications, autoimmune disorders, or genetic predisposition. That’s why awareness and early testing are just as important as prevention.

Ryan Brady
December 7, 2025 AT 11:24