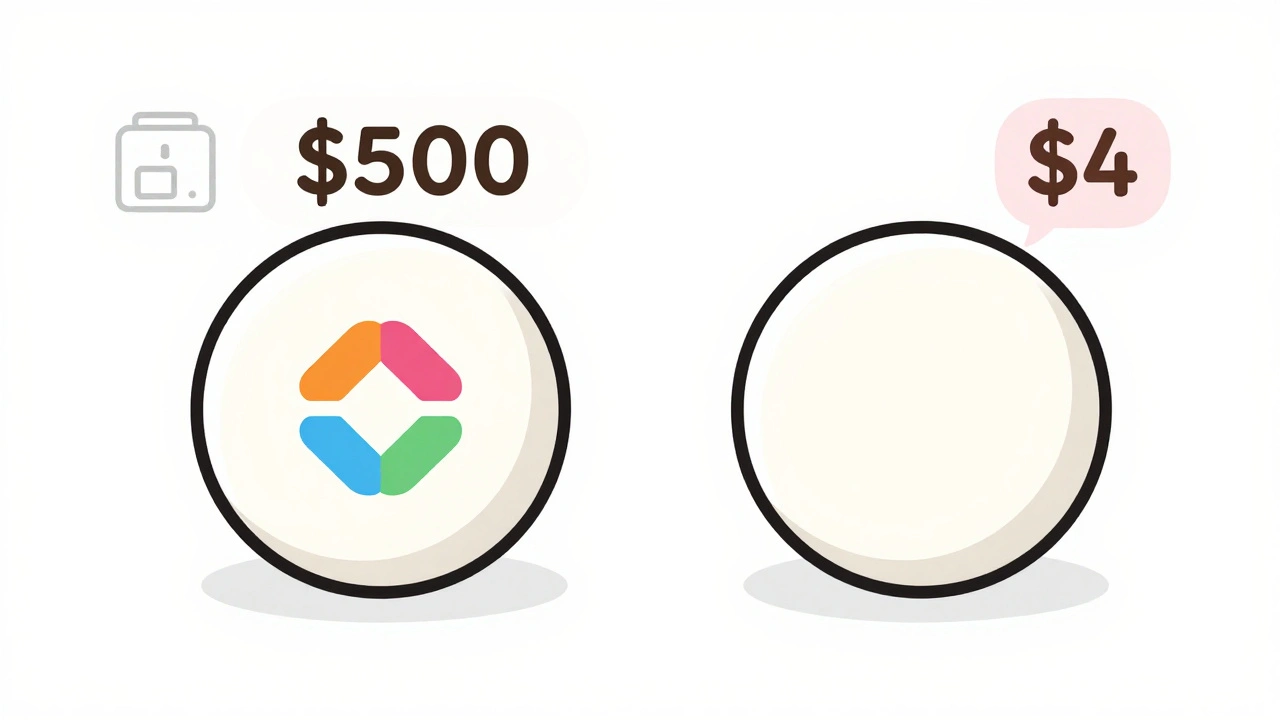
When you pick up a prescription, you might see two options: the familiar brand-name pill with the flashy logo, or a small, plain tablet with a different color and shape. The brand-name version could cost $500 a month. The generic? $4. That’s not a typo. It’s not a scam. And it’s not magic. It’s the system working exactly as it was designed to.
Same medicine, different price tag
Generic drugs aren’t cheaper because they’re weaker, older, or made in a basement. They’re the exact same medicine as the brand-name version. Same active ingredient. Same strength. Same way it works in your body. The FDA requires it. Every single generic must prove it delivers the same amount of medicine into your bloodstream at the same speed as the brand. That’s not a suggestion-it’s a legal requirement. If it doesn’t match within strict limits, it doesn’t get approved.So why the massive price difference? It comes down to one thing: who pays for the research.
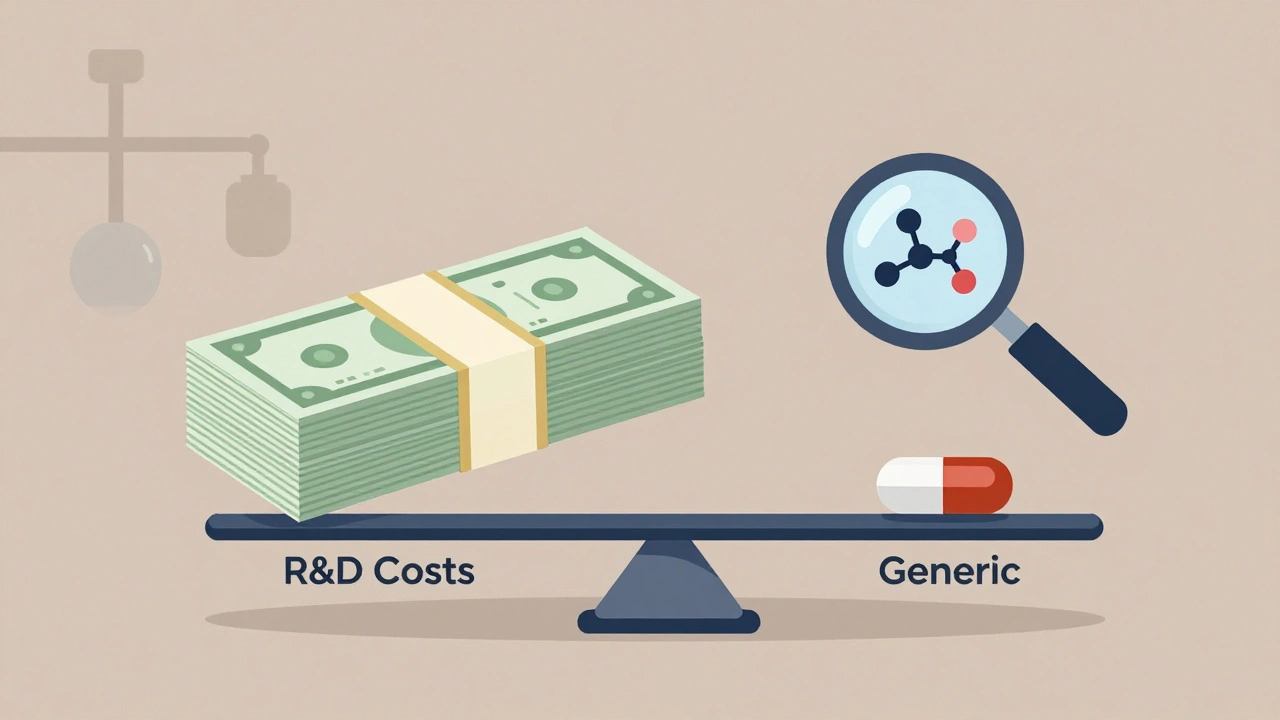
The $2.6 billion price of being first
Developing a new brand-name drug isn’t just expensive-it’s a marathon that takes 8 to 12 years. Companies spend an average of $2.6 billion to take a drug from lab to pharmacy shelf. That includes testing on animals, running clinical trials with thousands of people, navigating regulatory reviews, and covering the cost of drugs that fail along the way. Most drugs never make it. For every one that gets approved, dozens get scrapped.That’s why brand-name companies charge so much. They’re not just selling medicine. They’re trying to recover years of investment, pay back investors, and fund the next round of research. They get 20 years of patent protection from the moment they file the patent. That’s their monopoly window. No one else can legally make the drug until that clock runs out.
How generics skip the cost
Generic manufacturers don’t have to do any of that. Once the patent expires, they can step in. They don’t need to repeat the animal tests or the massive human trials. Instead, they file what’s called an Abbreviated New Drug Application (ANDA). All they need to prove is that their version is bioequivalent to the brand. That means matching the absorption rate and blood concentration levels within a narrow range. It’s faster. It’s cheaper. And it costs about $1 to $5 million per drug-less than 0.2% of what the brand company spent.The FDA doesn’t cut corners on quality. Generics are held to the same manufacturing standards as brand-name drugs. The same clean rooms. The same inspections. The FDA checks around 12,000 manufacturing sites worldwide every year. Whether it’s made in the U.S., India, or Germany, the rules are identical. The only differences you’ll see are in the color, shape, or flavor-things that don’t affect how the drug works. Those are changed to avoid trademark issues.
Competition drives prices down
Once the first generic hits the market, the price drops fast. Usually by 80% or more within the first year. Why? Because more companies jump in. On average, 14 different manufacturers make the same generic drug. More suppliers mean more competition. More competition means lower prices. It’s basic economics.Take atorvastatin, the generic version of Lipitor. When Lipitor’s patent expired, dozens of companies started making it. Today, a 30-day supply costs $4. The brand version? Around $500. Omeprazole, the generic for Prilosec, runs $6 a month instead of $300. These aren’t outliers. They’re the norm.
Who’s saving money?
The biggest winners? Patients. Insurance companies. And the whole healthcare system.In the U.S., generics make up 90% of all prescriptions filled. But they account for only about 18% of total drug spending. That means brand-name drugs-just 10% of prescriptions-are eating up 82% of the money. That’s why your insurance plan pushes generics. They’re Tier 1 on most formularies, meaning your copay might be $0 to $15. Brand-name drugs? $25 to $50. Specialty drugs? You might pay 25% of the cost-sometimes hundreds of dollars.
From 2007 to 2016, generics saved the U.S. healthcare system over $1.67 trillion. In 2022 alone, they saved $293 billion. That’s not just pocket change. That’s billions of dollars that didn’t go to drug companies. It’s money that stayed in people’s wallets, kept premiums lower, and kept care affordable.
Why do people still hesitate?
Even with all the proof, many people still worry. A 2023 survey found that 62% of Americans trust brand-name drugs more-even though 84% admit generics work just as well. Some of that comes from looks. A generic pill might be a different color or shape. If you’ve been taking a blue pill for years and suddenly get a white one, it’s natural to wonder if something changed.There’s also misinformation. Some patients report side effects after switching. But in most cases, those symptoms were already there. Or they’re caused by changes in inactive ingredients-like fillers or dyes-that don’t affect how the drug works. Rarely, for drugs with a very narrow therapeutic index-like warfarin or levothyroxine-some doctors prefer to stick with one brand or generic to avoid even tiny variations. But the FDA says all approved generics are safe and effective.
Pharmacists are trained to explain this. Most states allow them to substitute a generic unless the doctor says no. A good pharmacist will spend 3 to 5 minutes walking you through the switch-showing you the new pill, confirming it’s the same medicine, and answering questions.

What’s next?
The pipeline for generics is growing. In 2022, the FDA approved over 1,000 new generics. More than 150 brand-name drugs are set to lose patent protection by 2028, with combined sales of $157 billion. That means even more savings coming. The FDA is also speeding up approvals for complex generics-like inhalers and topical creams-that used to take years to get approved. Now, they’re aiming for half the time.And it’s not just pills. Biosimilars-generic versions of complex biologic drugs-are starting to enter the market. These are harder to copy than regular pills, but they’re coming. By 2028, they could save billions more.
What you can do
If you’re on a brand-name drug and paying a lot:- Ask your doctor if a generic is available.
- Check with your pharmacist-they know what’s covered and what’s cheapest.
- Use tools like GoodRx or RxOutreach to compare prices.
- Don’t assume brand = better. The science says otherwise.
Switching to a generic doesn’t mean lowering your standards. It means making a smarter choice. You’re getting the same medicine. Just without the marketing bill.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they deliver the same amount of medicine into your bloodstream at the same rate. This is called bioequivalence. Thousands of studies and decades of real-world use confirm that generics work just as well.
Why do generic pills look different?
By law, generic manufacturers can’t copy the exact appearance of brand-name pills to avoid trademark infringement. That’s why color, shape, or size might be different. But these changes don’t affect how the drug works. Only the active ingredient matters for effectiveness. The inactive ingredients-like fillers or dyes-are regulated and safe.
Can I switch from a brand to a generic safely?
For most medications, yes. The FDA and major medical groups like the American Medical Association support switching. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-some doctors prefer to stick with one version to avoid even small changes in blood levels. But that’s rare. If you’re concerned, talk to your doctor or pharmacist before switching.
Why are some generics more expensive than others?
Price differences between generics happen because of supply and demand. If only one company makes a certain generic, it might cost more. When multiple manufacturers enter the market, prices drop fast. Insurance formularies also influence price-some plans favor certain generic brands. Always check with your pharmacy or use a price-comparison tool like GoodRx.
Are generic drugs made in lower-quality factories?
No. The FDA inspects all manufacturing facilities-whether they make brand-name or generic drugs-using the same strict standards. Many brand-name companies actually make their own generics after the patent expires. The FDA conducts about 12,000 inspections annually worldwide. A generic drug made in India or China is held to the same quality rules as one made in the U.S.
Do insurance plans encourage generics?
Yes. Most insurance plans have three tiers: Tier 1 is generics (lowest cost), Tier 2 is brand-name drugs, and Tier 3 is specialty drugs. Generics usually have the lowest copay-sometimes $0. If you ask for the brand-name version when a generic is available, your insurance may deny coverage unless your doctor gets prior approval. This isn’t a trick-it’s how they keep costs down for everyone.
What if I feel different after switching to a generic?
It’s rare, but some people report changes in how they feel. This could be due to differences in inactive ingredients, stress from the switch, or unrelated health changes. If you notice new side effects or symptoms, talk to your doctor. Don’t stop taking the medication. Your pharmacist can help determine if it’s the drug or something else. In most cases, switching back or trying a different generic brand resolves the issue.
Anna Roh
December 9, 2025 AT 21:45