Venlafaxine Blood Pressure Risk Calculator
Blood Pressure Risk Assessment
This tool helps you understand your blood pressure risk while taking venlafaxine based on current clinical guidelines.
When you start taking venlafaxine for depression or anxiety, your doctor focuses on your mood, sleep, and energy levels. But there’s another number they’re watching closely - your blood pressure. Unlike many other antidepressants, venlafaxine doesn’t just change how your brain feels. It can also raise your blood pressure, sometimes significantly. This isn’t a rare side effect. It’s a well-documented, dose-dependent risk that needs real attention.
Why Venlafaxine Raises Blood Pressure
Venlafaxine is an SNRI - a serotonin-norepinephrine reuptake inhibitor. That means it boosts two brain chemicals: serotonin, which helps with mood, and norepinephrine, which affects alertness, focus, and your heart. The key here is norepinephrine. When it builds up in your system, it tightens blood vessels and makes your heart beat harder. That’s how your blood pressure goes up.
This effect isn’t obvious at low doses. At 37.5 mg or 75 mg a day, most people see little to no change. But once you hit 150 mg per day, the norepinephrine effect kicks in harder. At doses above 300 mg, the risk jumps. One major study of over 3,700 people found that 13.1% of those on high-dose venlafaxine developed clinically high blood pressure, compared to just 5% on placebo. That’s more than double the risk.
Even more concerning? It doesn’t always follow the rules. There are case reports of young, healthy people - no history of high blood pressure - suddenly seeing readings like 210/170 mmHg after only 150 mg a day. That’s not a fluke. That’s a medical emergency. One person described it as a ‘headache that wouldn’t quit,’ followed by nosebleeds and blurred vision. Those are red flags.
How It Compares to Other Antidepressants
If you’ve tried an SSRI like sertraline or fluoxetine and it didn’t help, your doctor might turn to venlafaxine. And for good reason - it works better for treatment-resistant depression. But that benefit comes with a trade-off.
SSRIs rarely affect blood pressure. In fact, they’re often preferred for people with heart conditions because they’re safer. Venlafaxine? It’s the opposite. Studies show it raises diastolic pressure by 1-3 mmHg on average at lower doses, but up to 15 mmHg in some cases over time. Desvenlafaxine, its active metabolite, does the same thing - even at low doses.
Compared to older tricyclic antidepressants (TCAs), venlafaxine doesn’t cause dizziness from low blood pressure. But it doesn’t help with it either. TCAs can swing both ways - lowering or raising pressure. Venlafaxine? It only pushes it up. Duloxetine, another SNRI, has less impact on blood pressure. So if you need an SNRI but have concerns about hypertension, duloxetine might be a better fit.
Who’s at Highest Risk?
Not everyone on venlafaxine gets high blood pressure. But some people are far more likely to.
- People on doses above 150 mg/day - the risk climbs sharply here.
- Those with existing hypertension - even if it’s controlled, venlafaxine can push it out of range.
- People with heart disease or kidney problems - their bodies handle pressure changes less well.
- Those with a family history of high blood pressure - genetics play a role.
- Older adults - blood vessels stiffen with age, making them more sensitive to norepinephrine.
Here’s something surprising: a 2021 review found that venlafaxine doesn’t make preexisting hypertension worse - it just raises pressure in people who were previously normal. So if your BP was 110/70 before starting, it might climb to 140/90. That’s still a problem. You don’t need to have high blood pressure to develop it from this drug.
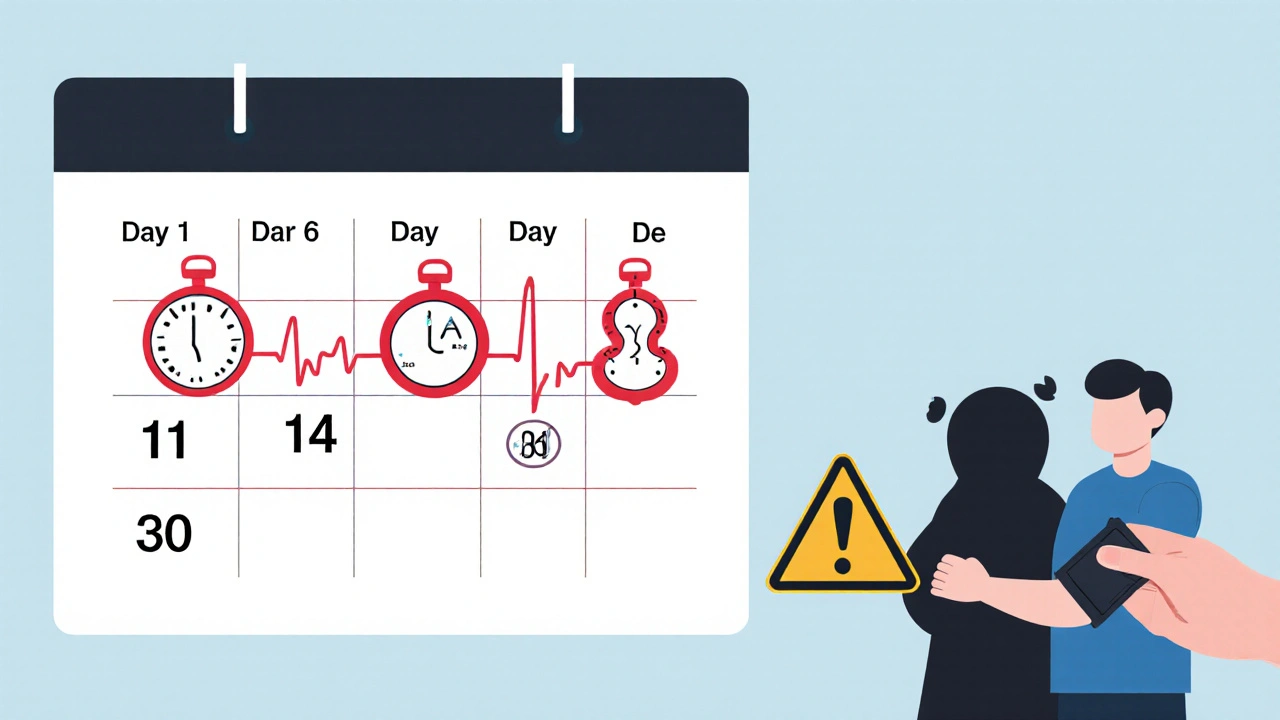
What Monitoring Actually Looks Like
It’s not enough to check your blood pressure once at your first appointment. You need a plan.
The American Psychiatric Association recommends:
- Baseline check - before you even start the medication.
- 2 weeks in - first follow-up to catch early spikes.
- 4 weeks in - confirm stability.
- Monthly for the first 3 months - if you’re on more than 150 mg/day.
- Quarterly after that - if your pressure stays stable.
Some doctors skip this. Don’t let them. If you’re taking venlafaxine and no one’s checking your BP regularly, you’re at risk. A 2023 Mayo Clinic guideline says this isn’t optional - it’s standard care.
And don’t wait for symptoms. High blood pressure doesn’t always cause headaches, nosebleeds, or chest pain. Many people feel fine - until they have a stroke or heart attack. That’s why regular checks matter more than how you feel.
What to Do If Your Blood Pressure Rises
If your BP climbs above 140/90 mmHg, talk to your doctor. Don’t panic. Don’t stop cold turkey. But don’t ignore it either.
Here’s what usually happens next:
- Dose reduction - dropping from 225 mg to 150 mg often brings pressure back down.
- Switching medications - many people switch to an SSRI or duloxetine with no loss of antidepressant effect.
- Adding a blood pressure med - sometimes, a low-dose beta-blocker or ACE inhibitor helps, but this isn’t ideal long-term.
- Stopping venlafaxine - if pressure stays high or climbs above 160/100, stopping is the safest move.
In most cases, blood pressure returns to normal within 1-4 weeks after stopping. One Reddit user shared: ‘I stopped at 37.5 mg after 2 months. My BP went from 155/102 to 120/80 in three weeks.’ That’s the pattern.
But if your systolic pressure hits 180 or diastolic hits 110 - that’s a hypertensive crisis. Go to the ER. Don’t wait. This can cause brain swelling, kidney damage, or heart failure.
Real People, Real Stories
Online forums are full of stories that textbooks don’t capture.
On PsychForums, 68% of users reported higher blood pressure on venlafaxine. One wrote: ‘I went from 118/76 to 152/98 in three weeks. My doctor said it was ‘just a little high’ - but I felt like my head was going to explode.’
On Drugs.com, 28% of negative reviews mention hypertension. One person said: ‘I took it for anxiety. My BP climbed so high I had to quit. I didn’t realize it was the drug until my cardiologist said, ‘This is venlafaxine-induced.’’
But not everyone has problems. A user on PatientsLikeMe with preexisting hypertension said: ‘Venlafaxine actually stabilized my BP.’ That’s rare, but it happens. Everyone’s body reacts differently.
The NHS says high blood pressure affects up to 1 in 10 people on venlafaxine. Serious cases? Less than 1 in 100. But when it happens, it can be life-threatening. That’s why monitoring isn’t just a suggestion - it’s a lifeline.
What This Means for You
If you’re on venlafaxine:
- Know your numbers. Keep a log - write down your BP readings every time you check.
- Ask your doctor: ‘Have you checked my blood pressure this month?’
- Don’t assume you’re fine because you feel good. Hypertension is silent.
- If you’re on more than 150 mg/day, monthly checks are non-negotiable.
- If your BP jumps, don’t wait. Call your doctor before your next appointment.
If you’re considering venlafaxine:
- Ask: ‘Is this the best choice for me, given my heart health?’
- Ask: ‘Have you checked my baseline BP?’
- Ask: ‘What’s the plan if my pressure goes up?’
Venlafaxine is powerful. It helps people who’ve tried everything else. But power comes with responsibility. Your mental health matters. So does your heart. You don’t have to choose one over the other - you just need to be watched.
Final Thought
This isn’t about scaring you off venlafaxine. It’s about making sure you’re safe while using it. Millions take it without issue. But thousands don’t. And for those who do, the difference between a simple dose adjustment and a stroke is often just one missed blood pressure check.
Don’t let your depression treatment become a hidden danger. Stay informed. Stay monitored. Your future self will thank you.
Can venlafaxine cause high blood pressure even at low doses?
Yes. While the risk is higher at doses above 150 mg/day, there are documented cases of severe hypertension - including readings over 200/100 mmHg - in people taking as little as 75 mg or 150 mg daily. These are rare, but they happen. Blood pressure changes can occur even in young, healthy people with no prior history of hypertension.
How often should I check my blood pressure on venlafaxine?
Baseline checks are required before starting. After that, check at 2 weeks and 4 weeks. If you’re taking more than 150 mg/day, monthly checks for the first 3 months are recommended. After that, quarterly checks are sufficient if your blood pressure is stable. Home monitoring is encouraged - don’t rely only on clinic visits.
Does venlafaxine make existing high blood pressure worse?
Studies show venlafaxine doesn’t necessarily worsen controlled hypertension - it raises pressure in people who were previously normal. But if your blood pressure is already high, even a small increase can push you into a dangerous range. That’s why monitoring is critical if you have preexisting hypertension.
What are the symptoms of venlafaxine-induced hypertension?
Many people have no symptoms. But warning signs include severe headaches, blurred vision, nosebleeds, chest pain, shortness of breath, or dizziness. If your systolic blood pressure hits 180 mmHg or diastolic hits 110 mmHg, seek emergency care immediately - this is a hypertensive crisis.
Can I switch from venlafaxine to another antidepressant if my blood pressure rises?
Yes. Many people switch successfully to SSRIs like sertraline or fluoxetine, or to duloxetine, which has less impact on blood pressure. Stopping venlafaxine usually brings blood pressure back to normal within 1-4 weeks. Your doctor can help you taper safely and choose a suitable alternative.
Is venlafaxine safe for people with heart disease?
It’s not the first choice. The American Heart Association recommends venlafaxine only when SSRIs have failed, and only with strict blood pressure monitoring. If you have heart disease, uncontrolled hypertension, or a history of stroke, your doctor should consider safer alternatives first. The risk of sudden pressure spikes can trigger cardiac events.

robert cardy solano
November 20, 2025 AT 11:11