Fournier's Gangrene Risk Calculator
Assess Your Risk
This tool helps you understand your risk of Fournier's gangrene while taking SGLT2 inhibitors based on key medical factors. The FDA reports 1.9 cases per 100,000 patient-years. Early detection is critical - each hour of delay increases mortality by 9%.
When you’re managing type 2 diabetes, taking a medication like SGLT2 inhibitors can feel like a win-better blood sugar control, less weight gain, and real protection for your heart and kidneys. But there’s a rare, dangerous side effect you won’t hear much about: Fournier’s gangrene. It’s not common. But when it happens, it can kill you in days if you don’t act fast. This isn’t a scare tactic. It’s a reality backed by the FDA, the UK’s MHRA, and dozens of medical case reports. If you’re on one of these drugs, you need to know the warning signs-and what to do the moment they show up.
What Are SGLT2 Inhibitors?
SGLT2 inhibitors are a class of diabetes medications that work by making your kidneys flush out extra sugar through urine. That’s it. No insulin needed. The first one, canagliflozin (Invokana), got FDA approval in 2013. Since then, four others joined the list: dapagliflozin (Farxiga), empagliflozin (Jardiance), ertugliflozin (Steglatro), and a few generics. They’re popular because they don’t cause low blood sugar like some older drugs, and they’ve been shown to cut heart failure hospitalizations by up to 30% in high-risk patients.
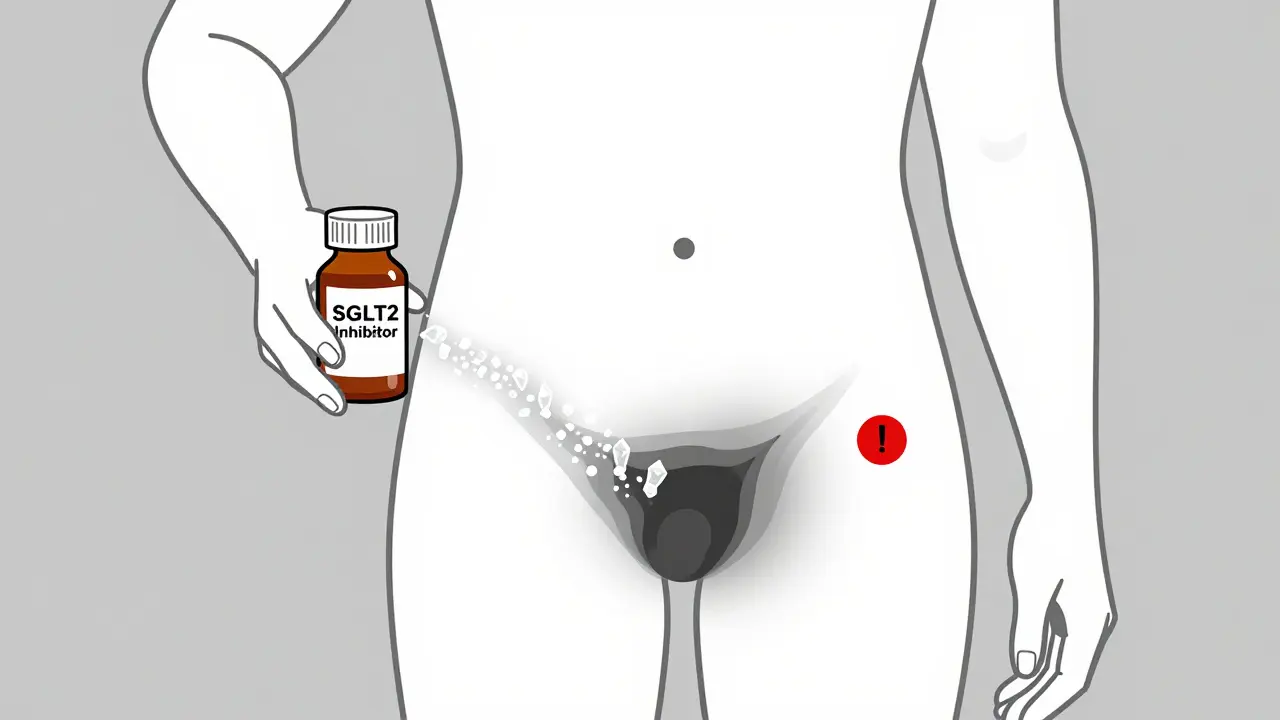
But here’s the catch: when sugar ends up in your urine, it doesn’t just disappear. It sticks around near your genitals and anus. Bacteria love sugar. And in some people, that creates the perfect storm for a rare, aggressive infection called Fournier’s gangrene.
What Is Fournier’s Gangrene?
Fournier’s gangrene is a type of necrotizing fasciitis-it’s not just a skin infection. It eats through the layers of tissue under your skin, starting in the genital or anal area. The bacteria involved are often a mix of E. coli, staph, and anaerobic bugs that normally live harmlessly in your gut. But when they get into the wrong place, they spread fast. Within hours, the tissue turns black. Swelling explodes. Fever spikes. Pain becomes unbearable.
It’s rare. But deadly. About 4 to 8% of people who get it die-even with surgery and antibiotics. And while it mostly affects men, about one-third of reported cases in Europe were in women. That’s important. This isn’t just a male problem.
The Link Between SGLT2 Inhibitors and Fournier’s Gangrene
The FDA first flagged this link in 2018 after 12 cases were reported between 2013 and 2018. That’s not a lot-but each case was severe. Since then, more have popped up. By 2024, the estimated risk was about 1.9 cases per 100,000 patient-years. That sounds tiny. But here’s the math: if 10,000 people take an SGLT2 inhibitor for a year, roughly one might develop Fournier’s gangrene. For comparison, the risk of a heart attack from stopping your blood pressure meds? Much higher. But this one? It’s silent. Fast. And avoidable-if you know what to look for.
Why does this happen? Three reasons:
- Sugar in urine = bacteria buffet
- High glucose levels weaken local tissue defenses
- Some evidence suggests these drugs may slightly dampen immune response in the genital area
And here’s something critical: almost all the reported cases involved people with poorly controlled diabetes. HbA1c above 9%. That’s not a coincidence. High blood sugar already weakens your immune system. Add sugar in your urine? That’s a double hit.
Early Warning Signs You Can’t Ignore
If you’re on an SGLT2 inhibitor, here’s your checklist of red flags. Don’t wait. Don’t think it’s a yeast infection or a pimple. Don’t brush it off. If you have any of these, go to the ER now:
- Sudden, severe pain in your genitals, perineum, or anus
- Swelling that spreads quickly-within hours
- Red, hot, or shiny skin that looks bruised or discolored
- Fever over 101°F (38.3°C)
- Malaise-feeling like you’re dying, even if you don’t know why
- Crackling under the skin (crepitus) when you touch the area
- Black or dead-looking skin patches
These symptoms don’t show up slowly. They explode. One day you feel fine. The next, you can’t sit down. That’s not normal. That’s an emergency.
What to Do If You Suspect Fournier’s Gangrene
Time is tissue. And tissue is life. If you think this is happening:
- Stop taking your SGLT2 inhibitor immediately.
- Call 911 or go to the nearest emergency room. Say: “I’m on an SGLT2 inhibitor and I think I have Fournier’s gangrene.”
- Don’t wait for a primary care appointment. Don’t call your pharmacist. Go now.
- Bring your medication bottle with you.
At the hospital, they’ll do a CT scan or ultrasound to check for gas in the tissue-signs of infection spreading under the skin. Blood tests will show infection markers. But the real treatment? Surgery and antibiotics. Fast. Within hours.
Each hour of delay increases your risk of death by about 9%. That’s not a guess. That’s from a 2022 study in Cureus. If you wait 24 hours, your survival odds drop sharply. This isn’t a “wait and see” situation.
Who’s at Highest Risk?
Not everyone on SGLT2 inhibitors will get this. But some people are more vulnerable:
- Men over 50 with diabetes
- People with HbA1c above 9%
- Those with a history of genital yeast infections or urinary tract infections
- People with obesity, poor hygiene, or weakened immune systems (from steroids, chemo, HIV, etc.)
- Anyone with recent genital trauma or surgery
Women are at lower risk-but not zero. One-third of cases in Europe were in women. Don’t assume it can’t happen to you.
Should You Stop Taking Your SGLT2 Inhibitor?
No-not unless you have symptoms. These drugs save lives. They reduce heart failure hospitalizations. They slow kidney disease. For most people, the benefits far outweigh the risk. The FDA, the American Diabetes Association, and the European Medicines Agency all still recommend them.
What you need is awareness, not fear. Talk to your doctor. Ask: “Am I at higher risk for this?” If your HbA1c is 7.5% and you’ve never had a yeast infection? You’re fine. If your HbA1c is 10.5% and you get urinary infections every few months? Maybe it’s time to reconsider.
But don’t quit cold turkey. Stopping suddenly can spike your blood sugar. Work with your provider to switch safely if needed.
What Doctors Are Doing Now
Since 2018, every SGLT2 inhibitor label has a boxed warning-the strongest type the FDA gives. Pharmacists are supposed to hand out patient guides. But many don’t. That’s why you need to be your own advocate.
Some clinics now use checklists before prescribing: “Have you had genital infections in the past year?” “Is your HbA1c under 8%?” “Do you have any immune issues?” If your doctor doesn’t ask, ask them.
Regulators are still tracking cases. The FDA’s FAERS system and the EU’s EudraVigilance database are collecting reports. So far, no new drugs in this class have been pulled. But the warning is clear: this is real. And it’s preventable-with knowledge.
Bottom Line: Stay Informed, Not Afraid
SGLT2 inhibitors are powerful tools. But like any tool, they come with risks. Fournier’s gangrene is rare. But it’s terrifying. And it doesn’t care if you’re young, old, male, or female. It only cares if you’re unaware.
If you’re on one of these drugs, keep your blood sugar under control. Practice good hygiene. Don’t ignore genital pain. And if something feels wrong-go to the ER. Don’t wait. Don’t call your doctor first. Go. Because in this case, seconds matter more than schedules.
You didn’t start this medication to risk your life. You started it to live better. Stay informed. Stay alert. And don’t let silence kill what you’re trying to protect.
Meghan Hammack
January 9, 2026 AT 01:55