Rhabdomyolysis Risk Calculator
This tool estimates your risk of developing rhabdomyolysis (dangerous muscle breakdown) based on common medication combinations and risk factors. Remember: most severe cases involve drug interactions, not single medications.
Imagine taking your daily statin for cholesterol, then adding an antibiotic for a sinus infection-and within days, your muscles ache like you ran a marathon, your urine turns dark brown, and you can barely stand up. This isn’t rare. It’s rhabdomyolysis, a dangerous muscle breakdown triggered by common drug combinations, and it’s happening more than you think.
What Exactly Is Rhabdomyolysis?
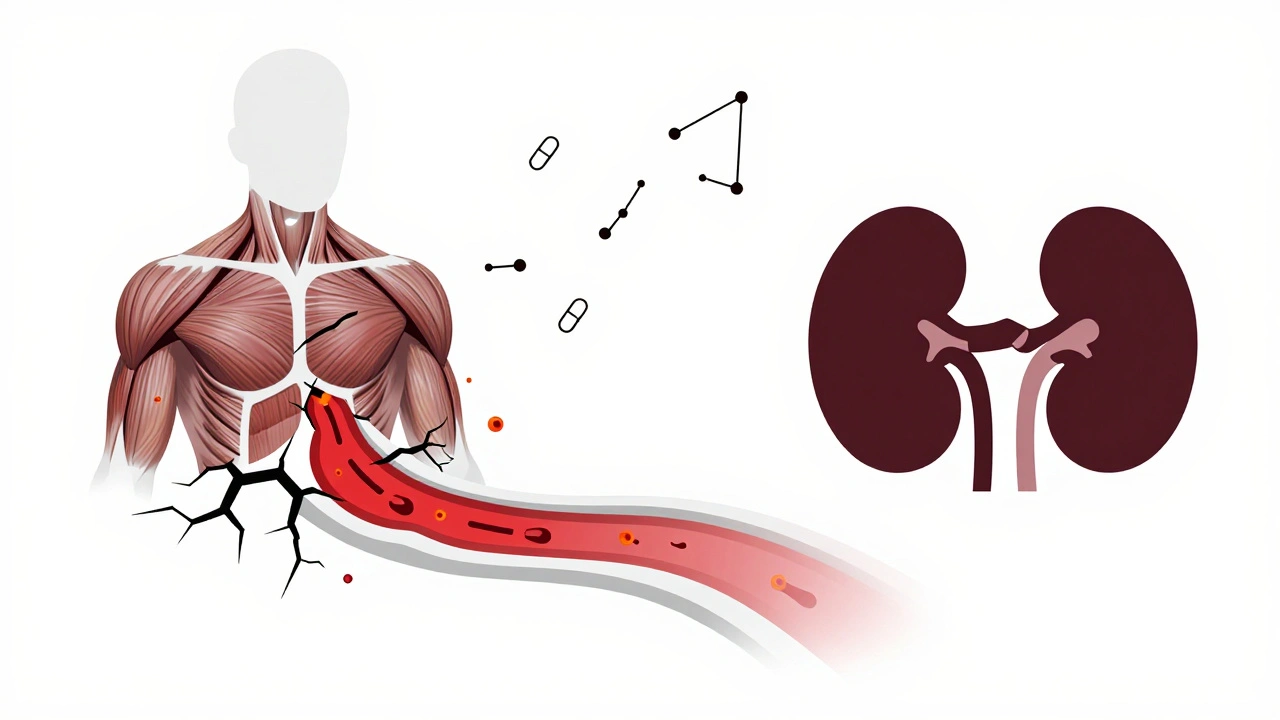
Rhabdomyolysis isn’t just sore muscles. It’s when muscle cells rupture and dump their contents-like creatine kinase, potassium, and myoglobin-into your bloodstream. Myoglobin is especially dangerous. It clogs your kidneys, leading to acute kidney injury. Up to half of people with severe rhabdomyolysis end up needing dialysis. About 5 to 15% of these cases are fatal, especially if kidney failure kicks in.
It’s not always obvious. The classic signs-muscle pain, weakness, and dark urine-only show up in about half the cases. Many people just feel tired, nauseous, or have vague abdominal pain. By the time they go to the ER, their creatine kinase (CK) levels are already over 10,000 U/L. Normal is under 200. Levels above 5,000 mean serious muscle damage.
Statins Are the Main Culprit-But Only When Combined
Statins like atorvastatin (Lipitor) and simvastatin (Zocor) are responsible for nearly 60% of all drug-induced rhabdomyolysis cases. But here’s the key: most of those cases happen because of interactions, not the statin alone.
Simvastatin, especially, is a ticking time bomb when mixed with certain drugs. Take clarithromycin, a common antibiotic. When combined with simvastatin, the risk of rhabdomyolysis jumps 18.7 times. Why? Both drugs are processed by the same liver enzyme-CYP3A4. When one blocks it, the other builds up to toxic levels in your blood.
Other dangerous combos:
- Simvastatin + gemfibrozil (a cholesterol drug): 15 to 20 times higher risk
- Colchicine (for gout) + clarithromycin or azole antifungals: 14 times higher risk
- Erlotinib (a cancer drug) + simvastatin: CK levels over 20,000 U/L reported in days
Even over-the-counter supplements like red yeast rice-which contains a natural statin-can trigger this when taken with prescription statins. Many patients don’t even realize they’re doubling down on the same drug class.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop rhabdomyolysis from medications:
- People over 65: 3.2 times more likely
- Women: 1.7 times more likely than men
- Those with kidney problems (eGFR under 60): 4.5 times higher risk
- Anyone taking five or more medications: 17.3 times higher risk
One patient story from Mayo Clinic’s forum says it all: “I was on colchicine for gout, then got a sinus infection. My doctor gave me clarithromycin. Two days later, my urine looked like cola. CK was 28,500. I spent three days in the hospital.”
And here’s the scary part: 92% of patients in a Reddit survey said their doctors never warned them about these interactions. Pharmacists often catch it-but if the prescription goes through without a flag, it’s on the patient to know.
Other Medications That Can Trigger It
Statins aren’t the only offenders. Other drugs can cause rhabdomyolysis on their own-or worse, when stacked together:
- Colchicine: Used for gout. Alone, it’s safe for most. But with antibiotics like clarithromycin, it becomes deadly. The European Medicines Agency issued a warning in 2021 after reviewing over 1,200 cases.
- Zidovudine: An HIV drug. In clinical studies, 12.3% of patients on this drug had CK levels over 10 times normal.
- Leflunomide: For rheumatoid arthritis. Rare, but when it happens, CK levels can hit 50,000 U/L. Plasma exchange is often needed because the drug sticks around in your body for weeks.
- Propofol: The anesthesia used in ICUs. Propofol infusion syndrome is rare, but when rhabdomyolysis develops, mortality hits 68%. It shuts down energy production in muscle cells.
Even antivirals like remdesivir, used during the pandemic, triggered a 22.4% spike in rhabdomyolysis reports to the FDA’s monitoring system. No one expected it-but the data didn’t lie.
How Doctors Diagnose It
There’s no single test. Diagnosis relies on three things:
- CK levels: Above 1,000 U/L is the red flag. Above 5,000 means severe damage. Some cases hit 100,000.
- Symptoms: Muscle pain, dark urine, weakness, nausea, fever.
- Medication history: What’s been added or changed in the last 30 days? Over half of cases happen within a month of a new drug or dose change.
Doctors also check for electrolyte imbalances-high potassium, low calcium, and rising phosphate levels. These can cause heart rhythm problems. And if swelling in the limbs is present, they’ll look for compartment syndrome, where pressure builds and cuts off blood flow.

What Happens in the Hospital
If you’re admitted for rhabdomyolysis, the clock starts ticking. Treatment isn’t about fixing the muscle-it’s about saving your kidneys.
The Cleveland Clinic protocol is clear:
- Stop the offending drug immediately
- Give 3 liters of IV saline in the first 6 hours
- Then keep fluids going at 1.5 liters per hour
- Add sodium bicarbonate to keep urine pH above 6.5 (this stops myoglobin from clumping in kidneys)
Some patients need dialysis. Others need plasma exchange-especially if they’re on leflunomide. The goal? Flush out the toxins before they wreck your kidneys.
Recovery takes time. People without kidney damage usually feel better in 12 weeks. Those who needed dialysis? It can take six months or more. And 44% still have muscle weakness a year later.
How to Prevent It
You don’t have to wait for a crisis. Here’s how to stay safe:
- Always tell your doctor every medication you take-including supplements, OTC painkillers, and herbal products.
- Ask: “Could this drug interact with anything else I’m on?” Especially if you’re on statins, colchicine, or cancer drugs.
- Know your risk factors: Age, kidney function, number of meds. If you’re over 65 and on five drugs, you’re in the danger zone.
- Watch for early signs: Unexplained muscle soreness, dark urine, fatigue. Don’t brush it off as “just getting older.”
- Get a CK test if you’re on high-risk combos-especially if you’re starting a new drug.
Pharmacists are your allies. If you pick up a new prescription, ask: “Is this safe with my other meds?” Most pharmacies now run automated checks-but not all catch every interaction.
The Bigger Picture
This isn’t just about one drug or one interaction. It’s about polypharmacy-the reality that older adults are taking more and more pills. In 2022, people on five or more medications were 17 times more likely to develop drug-induced rhabdomyolysis. And that number is rising by over 8% each year.
Regulators are catching on. The FDA now requires statin labels to list specific contraindications with CYP3A4 inhibitors. The European Medicines Agency has tightened warnings on colchicine combos. But guidelines don’t always reach the front lines.
Meanwhile, researchers are working on solutions: genetic tests to spot people with the SLCO1B1*5 allele (who are 4.5 times more sensitive to simvastatin), and AI systems that flag dangerous combos before prescriptions are filled.
For now, the best protection is awareness. If you’re on a statin, and your doctor adds an antibiotic, antifungal, or painkiller-ask. Don’t assume it’s safe. Muscle breakdown doesn’t come with a warning label. It comes with pain, dark urine, and a hospital bed.
Can rhabdomyolysis happen from one medication, or only from interactions?
Rhabdomyolysis can happen from a single medication, but it’s rare. Most cases-especially severe ones-are caused by drug interactions. Statins alone can cause mild muscle pain in up to 10% of users, but full-blown rhabdomyolysis usually requires another drug that blocks how the body breaks it down. For example, simvastatin by itself has a very low risk. Add clarithromycin, and the risk jumps nearly 20 times.
How quickly does rhabdomyolysis develop after starting a new drug?
It usually happens within 30 days of starting a new medication or changing a dose. About half of cases occur in the first two weeks. Statin-related cases often appear around 28 days after starting the drug. But with strong interactions-like statin plus azole antifungal-symptoms can show up in as little as 48 hours.
Is it safe to take statins if I’m on other medications?
It depends. Statins are still the most effective way to lower heart attack risk. But not all statins are equal. Rosuvastatin and pravastatin are less likely to interact with other drugs because they’re not processed by the CYP3A4 enzyme. If you’re on a medication that inhibits CYP3A4-like clarithromycin, itraconazole, or grapefruit juice-your doctor may switch you to one of these safer options.
Can I check my CK levels at home?
No. Creatine kinase testing requires a blood draw and lab analysis. There are no reliable at-home tests. If you suspect rhabdomyolysis-dark urine, unexplained muscle pain, weakness-go to urgent care or the ER. Delaying treatment increases the risk of permanent kidney damage.
What should I do if I start feeling muscle pain while on a statin?
Don’t ignore it. Call your doctor and mention the pain, especially if it’s new, worsening, or accompanied by dark urine. Don’t stop the statin on your own-your doctor may want to check your CK level first. If it’s elevated, they’ll likely switch you to a different statin or adjust your other meds. Muscle pain isn’t always rhabdomyolysis, but it’s a signal to investigate.
Are there any supplements that increase the risk of rhabdomyolysis?
Yes. Red yeast rice contains monacolin K, which is chemically identical to lovastatin. Taking it with a prescription statin doubles your exposure. Other supplements like high-dose niacin, creatine (in rare cases), and some weight-loss products with stimulants have also been linked to muscle breakdown. Always tell your doctor what you’re taking-even if you think it’s “natural.”

patrick sui
December 2, 2025 AT 00:29