Renal Dosing Calculator
Renal Dosing Calculator
Results
Why Renal Dosing of Antibiotics Matters More Than You Think
When your kidneys aren’t working right, antibiotics can turn from lifesavers into dangers. It’s not about taking less medicine-it’s about taking the right amount. Too much and you risk seizures, hearing loss, or kidney damage. Too little and the infection won’t budge, leading to longer hospital stays, worse outcomes, or even death. This isn’t theory. In hospitals across the U.S., 22.7% of all antibiotic-related adverse events happen in patients with kidney disease. That’s more than one in five. And it’s preventable.
Here’s the hard truth: if you have chronic kidney disease (CKD), you’re not getting the same dose as someone with healthy kidneys. But most people don’t realize that. Even some doctors don’t adjust doses correctly. A 2023 survey found that 63% of physicians miscalculated kidney function using the Cockcroft-Gault equation. That’s not just a mistake-it’s a risk to life.
How Kidneys Handle Antibiotics-and Why That Changes Everything
Your kidneys filter blood. They remove waste, excess fluids, and drugs. About 60% of commonly used antibiotics are cleared mainly through the kidneys. That includes penicillins, cephalosporins, fluoroquinolones, and vancomycin. When kidney function drops, these drugs build up. And they don’t just sit there-they start attacking nerves, ears, and even the kidneys themselves.
Take vancomycin. It’s a go-to for serious infections like MRSA. But if your kidneys are failing and you get the standard 1,000 mg every 12 hours? You’re likely heading for toxicity. The drug accumulates. Your blood levels climb. You might develop red-man syndrome, kidney damage, or irreversible hearing loss. The fix? Lower the dose or extend the time between doses. But only if you know how much your kidneys are still doing.
That’s where creatinine clearance (CrCl) comes in. It’s not a fancy lab number. It’s your kidney’s actual filtering power. And it’s the single most important number when prescribing antibiotics in kidney disease.
CrCl: The Number That Saves Lives (And How to Calculate It)
The Cockcroft-Gault equation is still the gold standard-even in 2026. Why? Because it uses real-world data: age, weight, sex, and serum creatinine. The formula looks like this:
CrCl = [(140 - age) × weight (kg)] / [72 × serum creatinine (mg/dL)] × 0.85 (if female)
It’s not perfect. But it’s better than guessing. And it’s far more accurate than relying on estimated GFR (eGFR) alone, which was designed for tracking kidney disease progression-not dosing antibiotics.
Here’s what CrCl levels mean for dosing:
- Normal: CrCl >50 mL/min → standard dose
- Mild impairment: CrCl 31-50 mL/min → reduce dose by 25-50%
- Moderate impairment: CrCl 10-30 mL/min → reduce dose by 50-75%, extend interval
- Severe impairment or dialysis: CrCl <10 mL/min → use lowest effective dose, often every 24-48 hours
Don’t skip the weight adjustment. If someone is obese, use ideal body weight-not actual weight. Overestimating leads to overdosing. And overdosing in kidney disease is deadly.
Antibiotic Dosing by Type: What Works and What Doesn’t
Not all antibiotics behave the same. Some are forgiving. Others are razor-thin. Here’s how key ones are adjusted:
Ampicillin/Sulbactam
Standard: 1.5-3 g IV every 6 hours
CrCl 15-29 mL/min: 2 g every 12 hours
CrCl <15 mL/min: 2 g every 24 hours
Cefazolin
Standard: 1-2 g IV every 8 hours
CrCl <10 mL/min: 500 mg-1 g every 12-24 hours
Ciprofloxacin (oral)
Standard: 500 mg every 12 hours
CrCl 10-30 mL/min: 250 mg every 12 hours
CrCl <10 mL/min: 250 mg every 24 hours
Vancomycin
Standard: 15-20 mg/kg every 8-12 hours
CrCl <30 mL/min: 15-20 mg/kg every 24-48 hours (monitor trough levels)
Some antibiotics, like ceftriaxone, don’t need adjustment-even in severe kidney disease. That’s because they’re cleared through the liver. Giving less than the full dose here doesn’t help-it hurts. It lowers your chance of curing the infection.
The Big Mistake: Confusing Acute Kidney Injury (AKI) with Chronic Kidney Disease (CKD)
This is where most guidelines fail-and where patients get hurt.
Chronic kidney disease is stable. You know the numbers. You adjust once and stick with it. But acute kidney injury? That’s a rollercoaster. CrCl can drop in hours, then bounce back in days. Many hospitals apply the same dose reductions for AKI as they do for CKD. That’s dangerous.
Studies show that in AKI, unnecessary dose reduction increases treatment failure by 34%. Why? Because you’re starving the antibiotic of the concentration it needs to kill bacteria. Meanwhile, if the kidneys recover fast-say, in 48 hours-and you don’t ramp the dose back up, you risk toxicity.
Dr. Jason Roberts, lead author of the 2019 Clinical Infectious Diseases review, says it plainly: “Deferred renal dose reduction of wide therapeutic index antibiotics could improve outcomes.” Translation: Don’t cut the dose right away in AKI. Wait. Monitor. Adjust as needed.
What Hospitals Are Doing Right (And What They’re Still Getting Wrong)
Here’s the good news: 89% of U.S. hospitals now have electronic alerts that flag when a patient has low CrCl and an antibiotic needs adjustment. That’s huge. But alerts alone aren’t enough.
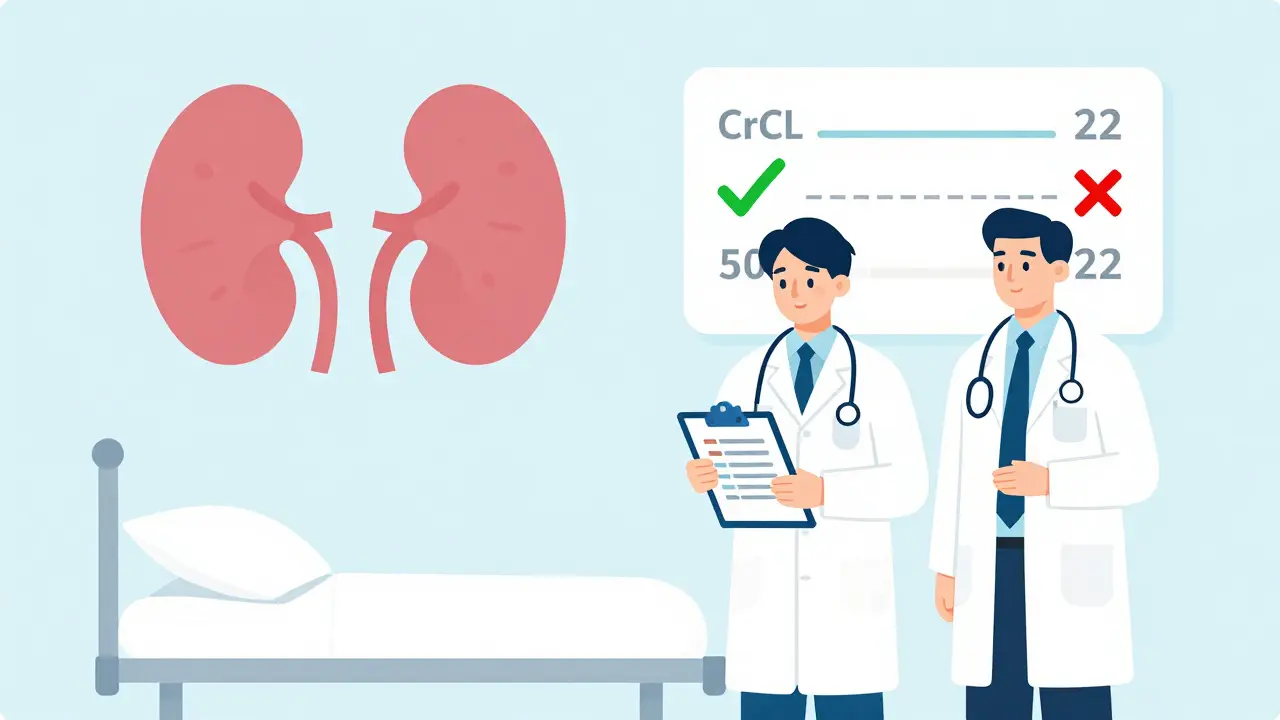
The real winners? Hospitals with pharmacist-led renal dosing teams. A 2021 study showed these teams cut antibiotic-related adverse events by 37%. Why? Because pharmacists check the math. They know the differences between UNMC, KDIGO, and Northwestern Medicine guidelines. They spot when a patient’s CrCl changed from 45 to 22 mL/min and the dose hasn’t been touched.
But here’s the problem: 41% of pharmacists say they struggle because guidelines conflict. For clarithromycin, UNMC says reduce if CrCl <30 mL/min. Northwestern says no change unless CrCl <50 mL/min. Which one do you follow?
Most academic centers standardize on KDIGO. It’s the most comprehensive. But even KDIGO doesn’t cover everything-especially augmented renal clearance (CrCl >130 mL/min). That’s when young, healthy, septic patients clear drugs so fast the standard dose doesn’t work. UNMC recommends 2 g IV every 4 hours for piperacillin/tazobactam in this group. Most guidelines don’t mention it.

What You Need to Do Now
If you’re a clinician:
- Calculate CrCl for every patient with suspected or known kidney disease-don’t assume.
- Use the Cockcroft-Gault equation. Don’t rely on eGFR alone for dosing.
- Know which antibiotics need adjustment. Don’t assume all do.
- For AKI, delay dose reduction. Reassess every 24-48 hours.
- Work with pharmacists. If your hospital doesn’t have a renal dosing team, push for one.
If you’re a patient or caregiver:
- Ask: “Is my kidney function checked before I get this antibiotic?”
- Ask: “Will my dose change if my kidneys are weak?”
- Ask: “Is this drug cleared by the kidneys?”
Don’t be shy. You’re not being difficult. You’re protecting your life.
The Future: AI, Monitoring, and Personalized Dosing
Things are changing. By 2027, 65% of academic hospitals plan to use therapeutic drug monitoring (TDM)-measuring actual drug levels in blood to guide dosing. That’s a game-changer for drugs like vancomycin and aminoglycosides.
AI dosing tools are already piloting in 17% of U.S. teaching hospitals. They pull in CrCl, weight, age, infection type, and even lab trends to suggest real-time adjustments.
And soon? We’ll see urinary biomarkers that tell us if kidneys are recovering-faster than waiting for creatinine to drop. That means we’ll stop underdosing patients who are healing.
The goal isn’t just to avoid toxicity. It’s to cure the infection-every time.
Frequently Asked Questions
Do all antibiotics need dose adjustments in kidney disease?
No. About 60% of commonly used antibiotics require adjustment because they’re cleared by the kidneys. But some, like ceftriaxone, linezolid, and metronidazole, are metabolized by the liver and don’t need changes-even in dialysis patients. Always check the specific drug’s profile before adjusting.
Can I use eGFR instead of Cockcroft-Gault for antibiotic dosing?
It’s not recommended. eGFR was designed to track chronic kidney disease progression, not to guide antibiotic dosing. The Cockcroft-Gault equation includes body weight and sex, which matter more for drug clearance. Using eGFR alone can lead to under- or overdosing. Stick with Cockcroft-Gault unless your hospital’s protocol says otherwise.
What if my creatinine level is normal but I have kidney disease?
Creatinine can stay normal even when kidney function is reduced-especially in older adults, people with low muscle mass, or those with advanced CKD. Never rely on creatinine alone. Always calculate CrCl using age, weight, sex, and creatinine. A normal creatinine doesn’t mean normal kidney function.
Should I give a loading dose in kidney disease?
Yes-for some drugs. Vancomycin, aminoglycosides, and certain beta-lactams need a loading dose to reach effective blood levels quickly, even in kidney disease. The maintenance dose is reduced, but the initial dose should still be full. Skipping the loading dose can delay treatment success.
How often should I recheck kidney function when adjusting antibiotics?
At least every 48 hours in acute kidney injury. In chronic kidney disease, check every 3-7 days if the patient is unstable or on multiple nephrotoxic drugs. If CrCl changes by more than 20%, reassess the antibiotic dose. Don’t set it and forget it.
Amit Jain
February 4, 2026 AT 08:49