NSAID & Blood Thinner Risk Calculator
This tool calculates the increased bleeding risk when combining NSAIDs with blood thinners based on the latest medical research. Using this information helps you make safer pain management choices.
Important Safety Notes
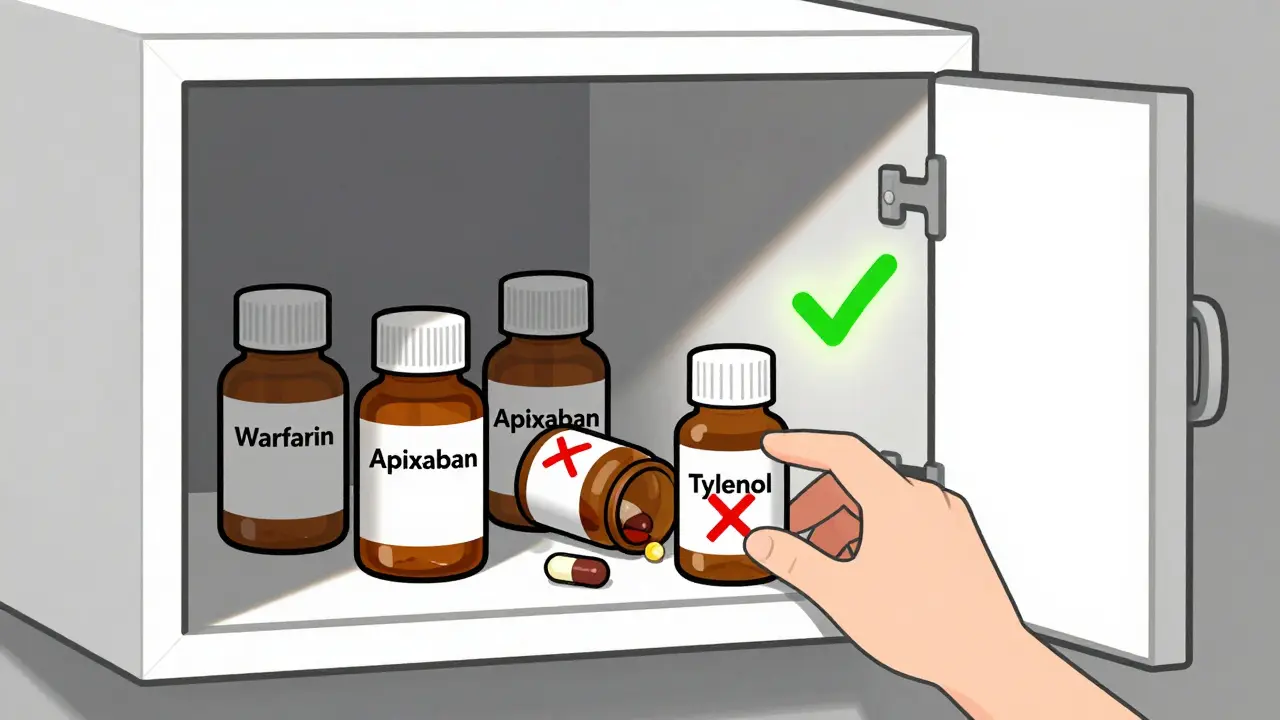
Never take NSAIDs if you're on blood thinners - The safest option is acetaminophen (Tylenol) at standard doses. If you accidentally took an NSAID, stop immediately and seek medical help if you experience any bleeding symptoms. Always check medication labels for hidden NSAIDs.
If you're taking a blood thinner like warfarin, apixaban, or rivaroxaban, and you reach for ibuprofen or naproxen for a headache or sore knee, you're putting yourself at serious risk. This isn't just a "be careful" warning-it's a life-threatening combination that sends tens of thousands of people to the emergency room every year. The truth is, many people don't even realize they're in danger because NSAIDs are sold over the counter, and pain is hard to ignore. But when these drugs mix with blood thinners, the result isn't just increased bruising-it's internal bleeding that can be fatal.
Why This Combination Is So Dangerous
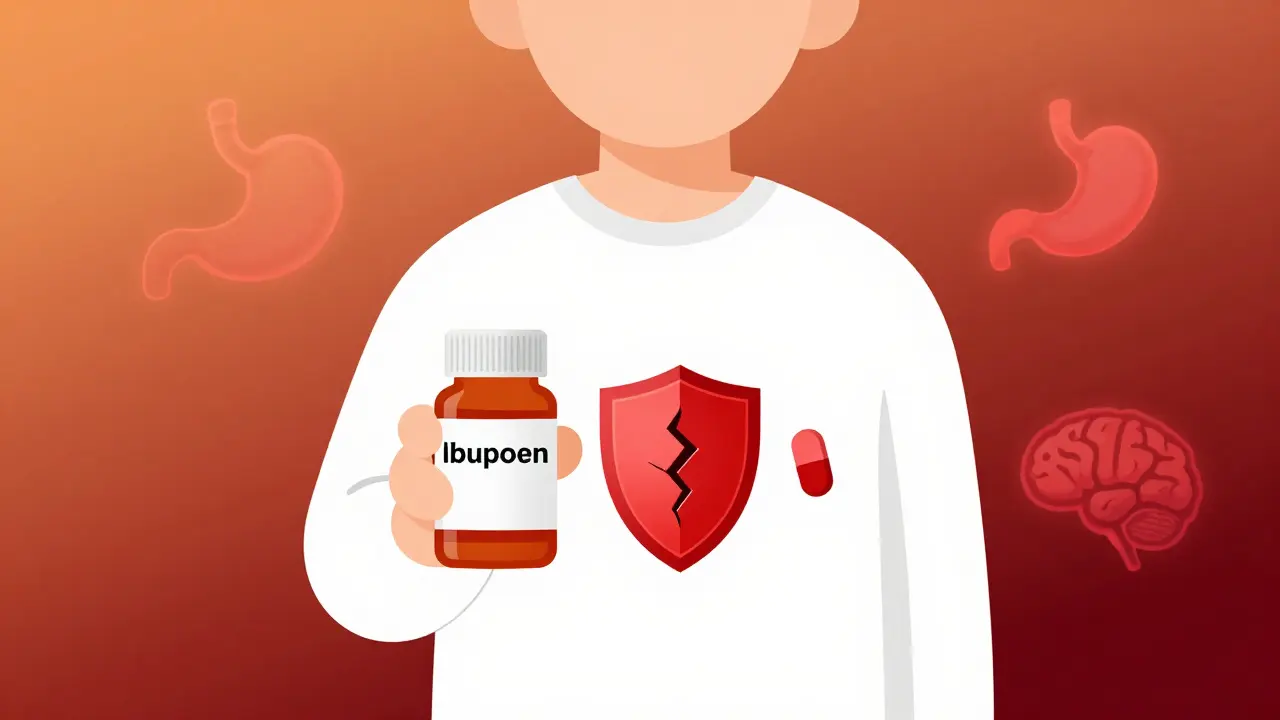
NSAIDs-like ibuprofen, naproxen, and diclofenac-work by blocking enzymes called COX-1 and COX-2. That reduces inflammation and pain, but it also messes with your platelets, the tiny blood cells that help clots form. Meanwhile, blood thinners like warfarin or the newer DOACs (direct oral anticoagulants) stop your blood from clotting too easily. When you take both, your body loses two layers of protection against bleeding. It’s like turning off both the brake and the emergency stop on a speeding car. The numbers don’t lie. A 2024 study from Denmark found that people on blood thinners who took NSAIDs had over twice the risk of serious bleeding compared to those who didn’t. That risk jumps even higher with certain NSAIDs: naproxen increases bleeding risk by 4.1 times, diclofenac by 3.3 times, and even ibuprofen by nearly 1.8 times. These aren’t small increases-they’re dramatic. The most common and deadly type of bleeding is in the stomach and intestines. Your gut lining gets damaged by NSAIDs, and blood thinners make it harder for your body to seal those wounds. Studies show a 2.24 times higher chance of gastrointestinal bleeding. That means vomiting blood, black tarry stools, or sudden weakness from internal blood loss. Intracranial bleeding-bleeding in the brain-is even more terrifying: risk goes up by 3.22 times. That’s not a typo. One fall, one bump, one sneeze too hard, and you could be in critical condition.Not All Blood Thinners Are the Same
Some people think all blood thinners are equal, but they’re not. Warfarin, the older drug, has the highest bleeding risk when mixed with NSAIDs-up to 3.8 times higher. Newer drugs like apixaban and edoxaban are safer overall, but they’re still dangerous with NSAIDs. The risk isn’t gone-it’s just lower. A 2022 study in the Journal of the American Heart Association showed that even with DOACs, NSAIDs still double the chance of bleeding. Here’s the breakdown:| Anticoagulant | Increased Bleeding Risk (HR) | 95% Confidence Interval |
|---|---|---|
| Warfarin | 3.8 | 3.2-4.5 |
| Dabigatran | 2.3 | 1.9-2.8 |
| Rivaroxaban | 2.1 | 1.8-2.4 |
| Apixaban | 1.9 | 1.6-2.3 |
| Edoxaban | 2.0 | 1.7-2.4 |
Even the "safer" NSAIDs aren’t safe. Celecoxib, a COX-2 inhibitor, is less likely to cause stomach bleeding than ibuprofen-but it still raises the risk by 1.4 times. And here’s the kicker: no NSAID is truly safe with any blood thinner. The American Heart Association, the American College of Cardiology, and the European Society of Cardiology all agree: avoid NSAIDs completely if you’re on long-term anticoagulation.
What Can You Take Instead?
The only widely accepted safe alternative is acetaminophen (Tylenol). At standard doses-up to 4,000 mg per day-it doesn’t interfere with platelets or clotting. Multiple studies confirm it doesn’t increase bleeding risk in people on warfarin or DOACs. That’s huge. For many, switching from ibuprofen to acetaminophen means less pain relief at first. But here’s the good news: a 2023 Cleveland Clinic study found that 68% of patients had adequate pain control after four weeks of switching to acetaminophen and adding physical therapy, heat, or massage. But acetaminophen isn’t perfect. If you have liver disease, drink alcohol regularly, or take other meds that affect the liver, even Tylenol can be risky. High doses cause liver failure. So stick to the label: no more than 3,000 mg if you’re over 65 or have liver issues. Other non-drug options work surprisingly well:- Physical therapy for joint pain-especially for arthritis
- Topical creams with menthol or capsaicin
- Heat wraps or cold packs
- Weight management to reduce stress on joints
- Low-impact exercise like swimming or walking
These aren’t just "nice to have"-they’re proven. A 2024 study in Health Affairs showed that patients in hospitals with antithrombotic stewardship programs (which include pain management education) reduced inappropriate NSAID use by 37%.
Hidden NSAIDs Are a Major Trap
Most people know ibuprofen and naproxen. But what about these?- Excedrin (contains aspirin)
- Midol (many versions have ibuprofen)
- DayQuil, NyQuil, and other cold/flu meds (check the label-it’s often listed as "ibuprofen" or "naproxen")
- Topical gels like Voltaren (diclofenac)
- Some arthritis patches and creams
On Reddit’s r/Anticoagulants, 62% of respondents admitted using NSAIDs with blood thinners. Of those, 38% had bleeding complications. Why? Because they didn’t realize their cold medicine had an NSAID. Or their dentist prescribed ibuprofen after a tooth extraction without knowing they were on apixaban. That’s not rare-it’s common. In fact, 15% of FDA reports on DOAC-related bleeding in 2022-2023 involved dental pain and NSAID use.
Always read the active ingredients. If you see "ibuprofen," "naproxen," "ketoprofen," "diclofenac," or "aspirin," don’t take it. Even if it’s "just one pill."
What If You Really Need an NSAID?
Sometimes, you have no choice. Maybe you had surgery, or you’re in severe pain and nothing else works. In those rare cases, the guidelines are clear:- Use the lowest possible dose-ibuprofen no more than 400 mg per day
- Take it for the shortest time possible-no longer than 3 days
- Always take a proton pump inhibitor (PPI) like pantoprazole (80 mg daily) to protect your stomach
- If you’re on warfarin, get your INR checked weekly during this time
This isn’t a suggestion-it’s the standard of care. But even with a PPI, you’re still at higher risk. A 2021 NIH study found that even with 78% of patients on PPIs, NSAID use still carried a bleeding risk. So this is damage control, not a green light.
Why Doctors Don’t Always Warn You
You’d think this would be obvious. But here’s the problem: only 41% of primary care providers consistently recommend acetaminophen over NSAIDs for patients on blood thinners. Only 22% refer patients to physical therapy. Why? Because pain is hard to manage, and doctors are under time pressure. Also, most electronic health records don’t block this combination. Only 38% of U.S. hospitals have automated alerts that stop a doctor from prescribing both. And patients? Only 29% remember being warned about NSAIDs three months after their doctor’s visit. That’s not your fault. It’s a system failure.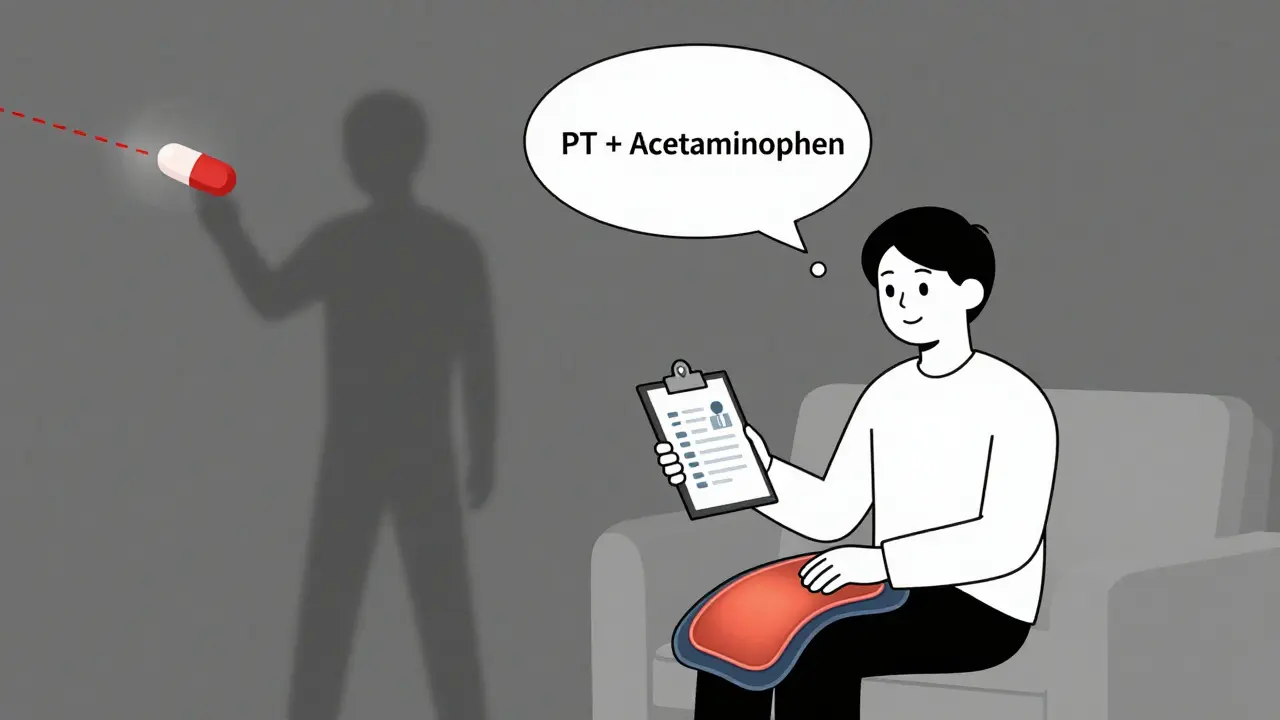
What You Should Do Right Now
If you’re on a blood thinner:- Check every medicine cabinet-throw out any NSAID-containing products you don’t need
- Read every OTC label before buying
- Ask your pharmacist: "Is this safe with my blood thinner?"-don’t assume they know your meds
- Tell every doctor, dentist, and specialist you’re on a blood thinner-before any procedure
- Switch to acetaminophen for pain, and ask about physical therapy or other non-drug options
Don’t wait for a bleeding episode to learn this lesson. The cost of these interactions in the U.S. is over $1.2 billion a year. That’s not just money-it’s hospital beds, emergency teams, and lives lost.
What’s Changing in 2025?
The American Heart Association is expected to release new guidelines in January 2025, likely strengthening the warning based on new data showing NSAIDs increase death risk by 1.8 times in people on anticoagulants. The FDA is pushing for AI tools that catch these dangerous combinations before they’re prescribed. And researchers are testing new NSAID formulas that don’t affect platelets-still in early trials, but promising.By 2030, experts predict a 50% drop in NSAID prescriptions for people on blood thinners, thanks to better alerts, better education, and better alternatives. But until then, the risk is real-and you’re the only one who can protect yourself.
Can I take ibuprofen if I’m on warfarin?
No. Ibuprofen increases your risk of serious bleeding by nearly 1.8 times when taken with warfarin. Even a single dose can raise your INR and lead to dangerous bleeding. Acetaminophen (Tylenol) is the safer choice for pain relief.
Is aspirin safe with blood thinners?
No. Aspirin is an NSAID and interferes with platelets. Even low-dose aspirin (81 mg) increases bleeding risk when combined with anticoagulants. Don’t take it unless your doctor specifically prescribes it for heart protection-and even then, it’s a calculated risk.
What’s the safest pain reliever with a blood thinner?
Acetaminophen (Tylenol) is the safest option at standard doses (up to 4,000 mg per day). It doesn’t affect clotting. But avoid it if you have liver disease or drink alcohol regularly. Always check with your doctor before starting any new medication.
Can I take NSAIDs occasionally if I’m on a DOAC?
It’s not recommended. Even newer blood thinners like apixaban or rivaroxaban still carry a doubled bleeding risk with NSAIDs. Occasional use isn’t safe-it’s a gamble. Use acetaminophen or non-drug methods instead.
How do I know if my cold medicine has an NSAID?
Look at the "Active Ingredients" list on the label. If you see ibuprofen, naproxen, diclofenac, ketoprofen, or aspirin, avoid it. Many cold medicines include these without making it obvious. When in doubt, ask your pharmacist.
What should I do if I accidentally took NSAIDs with my blood thinner?
Stop taking the NSAID immediately. Watch for signs of bleeding: unusual bruising, nosebleeds that won’t stop, dark or bloody stools, vomiting blood, severe headaches, or dizziness. Call your doctor or go to the ER if you notice any of these. Don’t wait.
josue robert figueroa salazar
December 25, 2025 AT 12:17