Every year, millions of people reach for ibuprofen or naproxen to ease a headache, back pain, or arthritic flare-up. These drugs work fast. They feel like a miracle. But behind the relief is a quiet danger most people never see - NSAID safety isn’t just about taking the right dose. It’s about knowing what your body is enduring while you’re feeling better.
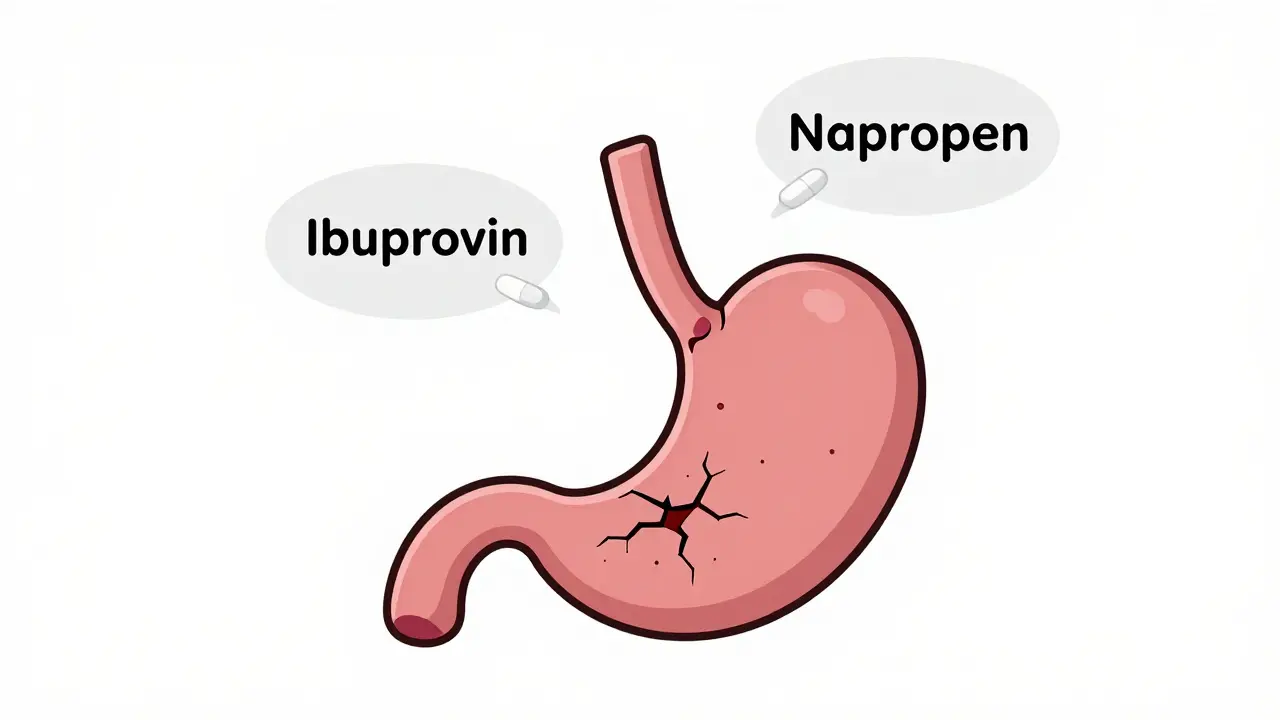
How NSAIDs Damage Your Stomach - Even When You Feel Fine
NSAIDs don’t just block pain signals. They shut down protective chemicals in your gut called prostaglandins. These aren’t just background players; they’re the body’s natural armor for the stomach and intestines. When you take an NSAID, you’re stripping away that armor - and the damage doesn’t always come with warning signs.Up to 50% of people who use NSAIDs long-term develop some level of stomach lining damage. But here’s the catch: half of those people won’t feel a thing until something serious happens - like internal bleeding. That’s not a myth. It’s what the American College of Gastroenterology found in their 2023 review. Many patients show up in the ER with black, tarry stools or extreme fatigue from blood loss - and they had no prior symptoms.
It’s not just the stomach. The small intestine gets hit too. NSAID-induced enteropathy is real. Studies in Gut and Liver show that even people who take NSAIDs for just a few weeks can develop tiny ulcers, inflammation, and bleeding in the lower gut. And unlike stomach ulcers, there’s no proven way to fully prevent or reverse this damage. That means if you’re on daily NSAIDs, your intestines are slowly being worn down.
Your Kidneys Are Also at Risk - Even If You’re Young and Healthy
People think kidney damage only happens to older adults with existing disease. That’s a dangerous assumption.NSAIDs reduce blood flow to the kidneys by blocking prostaglandins that help keep them functioning properly. In healthy people, this might just cause a small dip in kidney function - detectable only with a blood test. But in someone who’s dehydrated, on diuretics, or has even mild high blood pressure, this can trigger acute kidney injury. According to Kidney International Reports, 1% to 5% of NSAID users develop this condition within weeks of starting treatment.
Chronic use? That’s when things get worse. Long-term NSAID users face higher risks of interstitial nephritis, fluid retention, high blood pressure, and even kidney papillary necrosis - a rare but serious condition that destroys parts of the kidney tissue. The FDA now requires boxed warnings on all prescription NSAIDs specifically for kidney risks in patients over 65. But even younger adults aren’t safe. A 2023 Medicare analysis showed that nearly half of NSAID users under 65 never had their kidney function checked after starting the drug.
Not All NSAIDs Are Created Equal - Here’s What the Data Shows
If you’re choosing between ibuprofen, naproxen, or celecoxib, it’s not just about cost or availability. Risk levels vary significantly.Take upper GI bleeding. A 2023 meta-analysis in Clinical Pharmacology & Therapeutics found that naproxen increases your risk of bleeding by 4.2 times compared to someone not taking NSAIDs. Ibuprofen? It’s 2.7 times riskier than celecoxib. Celecoxib, a COX-2 inhibitor, cuts the GI bleeding risk in half - but it’s not risk-free. It still raises heart attack and stroke risk, especially in people with existing cardiovascular disease.
And here’s the twist: mixing NSAIDs with blood thinners, SSRIs, or corticosteroids multiplies the danger. One study in JAMA Internal Medicine showed that taking an SSRI with an NSAID increases bleeding risk by 3.38 times. That’s not a small bump. That’s a red flag.
Even OTC versions aren’t safe for daily use. The European Medicines Agency pulled high-dose diclofenac off the market in 2023 because of heart risks. And in the U.S., 30% of all NSAID prescriptions are for ibuprofen - the most commonly used, and one of the most dangerous when taken long-term.
Monitoring Isn’t Optional - It’s Lifesaving
You wouldn’t drive a car without checking the oil. Why treat your body any differently?The American Gastroenterological Association recommends checking your creatinine and blood urea nitrogen (BUN) within 30 days of starting an NSAID - and then every few months if you’re on it long-term. A simple blood test can catch early kidney trouble before it becomes irreversible.
For your gut? Fecal occult blood testing every six months is critical for high-risk patients. It detects hidden bleeding that no symptom can reveal. And if you’re over 65, have a history of ulcers, or are on multiple medications that increase bleeding risk, you should be using a validated risk calculator. Points add up fast: age over 65 = 2 points, prior ulcer = 3 points, anticoagulant use = 2 points. Four points or more? You’re in the high-risk zone. That means you need a plan - not just a pill.
Proton Pump Inhibitors (PPIs) - A Double-Edged Sword
Doctors often prescribe PPIs like omeprazole to protect the stomach when NSAIDs are necessary. And yes, they work - cutting ulcer risk by 70% to 90%. But here’s what most people don’t know: PPIs aren’t harmless.A 2022 study in PMC8002800 found that combining NSAIDs with PPIs for 4 to 12 months increases the risk of microscopic colitis - a chronic inflammatory bowel condition - by more than six times. That means you traded one problem for another. And PPIs don’t help your intestines at all. They leave your lower GI completely unprotected.
Dr. Kenneth W. Mahaffey of Stanford calls this the “therapeutic paradox.” You’re trying to fix one issue, but you’re creating new ones. And for many, the trade-off isn’t worth it.
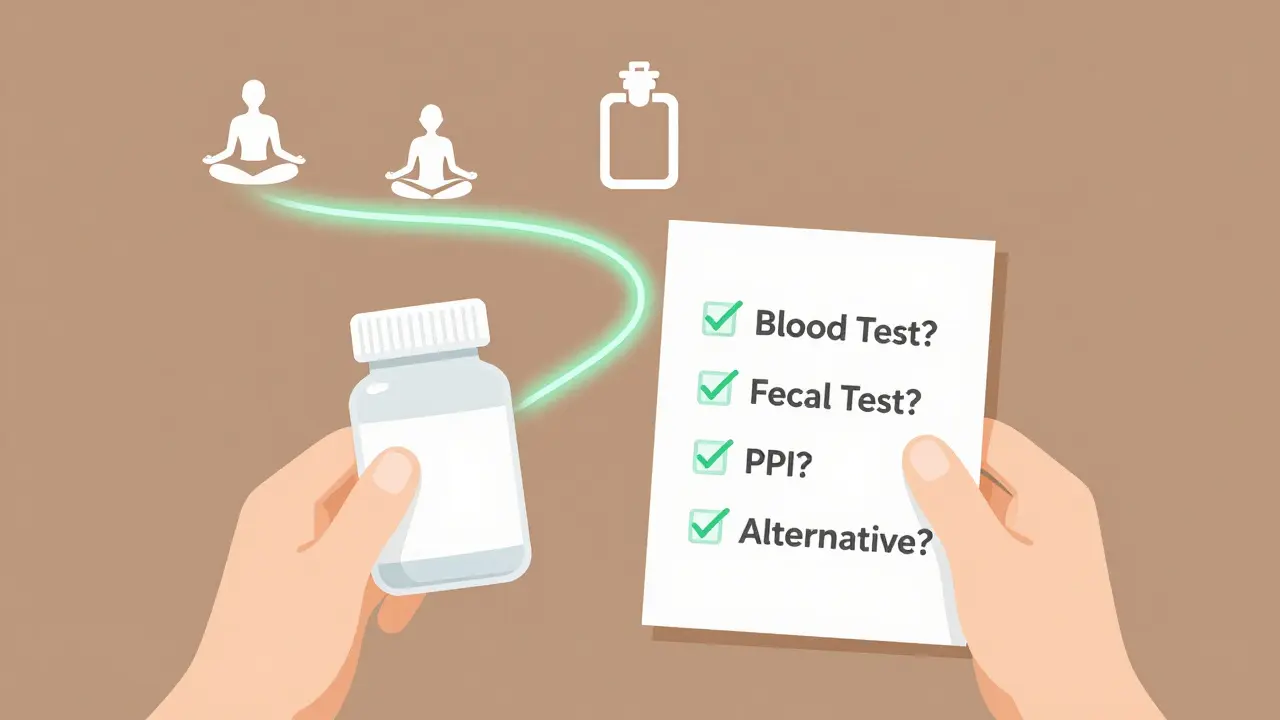
When to Stop - And What to Use Instead
The single most effective way to avoid NSAID complications? Don’t take them longer than you have to.Dr. Charlotte H. Clarke’s research shows that each extra week on NSAIDs increases your complication risk by 3% to 5%. That means a month of daily use isn’t “safe.” It’s a countdown.
If you’re on NSAIDs for chronic pain - like osteoarthritis - ask yourself: Is this the only option? Physical therapy, weight management, heat therapy, and even certain supplements like curcumin have shown promise in managing joint pain without systemic damage. For some, acetaminophen (Tylenol) is a safer short-term alternative - though it has its own liver risks if misused.
And if you must use NSAIDs? Use the lowest dose possible. Naproxen at 500 mg twice daily is far riskier than 250 mg once a day. And never combine different NSAIDs - not even an OTC and a prescription. That’s like doubling down on danger.
What Patients Are Saying - And Why It Matters
Real people are telling their stories. On Reddit, users report diarrhea lasting days after stopping naproxen. On WebMD, 42% of negative reviews mention sudden stomach bleeding with no warning. On Drugs.com, 22% of celecoxib users report leg swelling - a sign of fluid retention and possible kidney strain.One survey found that 57% of long-term NSAID users quit because of side effects. Not because the pain came back. Because they got sick. And many didn’t realize the drug was the cause until it was too late.
This isn’t about fear. It’s about awareness. You deserve pain relief - but not at the cost of your gut, your kidneys, or your future health.
The Future Is Changing - But You Can’t Wait
New drugs are coming. Naproxcinod, a newer NSAID that releases nitric oxide to protect the stomach lining, showed 58% fewer ulcers in trials. Point-of-care fecal tests for hidden bleeding are now 92% accurate. AI is being trained to spot early signs of intestinal damage during endoscopies.But these aren’t available everywhere. And even if they were, they’re not magic. The core truth hasn’t changed: NSAIDs are powerful tools - but they’re not harmless. The safest choice is still the one you make before you ever take the first pill.
Can I take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and reduce the effectiveness of many blood pressure medications. If you have hypertension, avoid long-term NSAID use. Talk to your doctor about alternatives like acetaminophen or non-drug therapies. If NSAIDs are necessary, monitor your blood pressure closely and avoid high doses.
Is it safe to take ibuprofen every day for arthritis?
No. Daily ibuprofen use increases your risk of stomach ulcers, kidney damage, and heart problems. Even at OTC doses, taking it every day for more than 10 days is not recommended. For chronic arthritis, work with your doctor to find a long-term plan that includes physical therapy, weight control, or safer medications like COX-2 inhibitors with protective agents.
Do I need a stomach protector if I take NSAIDs occasionally?
If you’re taking NSAIDs only once in a while - like for a headache or a sprained ankle - you likely don’t need a stomach protector. But if you’re using them more than twice a week for more than a month, you’re in the high-risk zone. At that point, talk to your doctor about whether a proton pump inhibitor (PPI) is right for you - and be aware that PPIs carry their own long-term risks.
What blood tests should I get if I’m on NSAIDs long-term?
You should have a basic metabolic panel (to check creatinine and BUN) every 3 to 6 months. A complete blood count (CBC) is also important to catch hidden bleeding - low hemoglobin or iron levels can signal internal blood loss. For high-risk patients, fecal occult blood testing every 6 months is strongly recommended.
Are there safer alternatives to NSAIDs for chronic pain?
Yes. For joint pain, physical therapy, weight loss, and heat/cold therapy are effective. Some people benefit from topical NSAIDs (like gels), which have far less systemic absorption. Acetaminophen is safer for the stomach and kidneys (but not the liver). Newer options include duloxetine for nerve-related pain, and in some cases, low-dose corticosteroid injections. Always discuss alternatives with your provider - don’t assume NSAIDs are the only option.
Christina Widodo
January 11, 2026 AT 19:02