More than two in three pregnant people experience nausea and vomiting - not just in the morning, but all day, every day. For many, it’s more than discomfort; it’s exhaustion, dehydration, and the inability to keep food down. The good news? There are safe, effective options. The tricky part? Not all medications are created equal. Some help without risk. Others carry hidden dangers you might not hear about until it’s too late.
First-Line Treatments: What Works Without Risk
The safest place to start is with what’s been used for decades - and studied the most. Pyridoxine (vitamin B6) at 25 mg three times a day is the gold standard. It’s not a miracle cure, but it’s better than placebo, and it doesn’t cross the placenta in harmful amounts. Add doxylamine (found in Unisom) at 25 mg at bedtime, and you’ve got the combination that makes up Diclegis - the only FDA-approved medication specifically for pregnancy nausea. This combo has been studied in over 1,000 pregnancies with no increase in birth defects. It’s not flashy, but it works.
And then there’s ginger. Not just a spice, but a proven treatment. Taking 250 mg of ginger root extract four times daily cuts nausea by more than half, according to a 2023 meta-analysis. One study of 77 pregnant women found ginger worked better for nausea, while pyridoxine was better for stopping vomiting. Many people prefer ginger because it doesn’t make them sleepy. On Reddit, 78% of users said ginger gave them moderate to full relief. Amazon reviews average 4.3 out of 5 stars. Sure, some complain about the taste - but no one’s reporting birth defects.
Antihistamines: The Quiet Workhorses
If B6 and ginger aren’t enough, antihistamines step in. Meclizine (Antivert), dimenhydrinate (Dramamine), and diphenhydramine (Benadryl) are all considered safe in pregnancy. Dosing is simple: 25-50 mg every 4-6 hours as needed. These were once thought to cause birth defects, but decades of data now say otherwise. AAFP’s 2003 review cleared meclizine specifically, and studies since then confirm it’s one of the most reliable options for nausea that doesn’t respond to first-line treatments.
They do come with side effects - mostly drowsiness. That’s why many people take them at night. One user on Drugs.com wrote, “I can finally eat breakfast, but I’m asleep by 10 a.m.” For some, that trade-off is worth it. For others, it’s a dealbreaker. The key is timing: take these before symptoms hit, not after you’ve already thrown up.
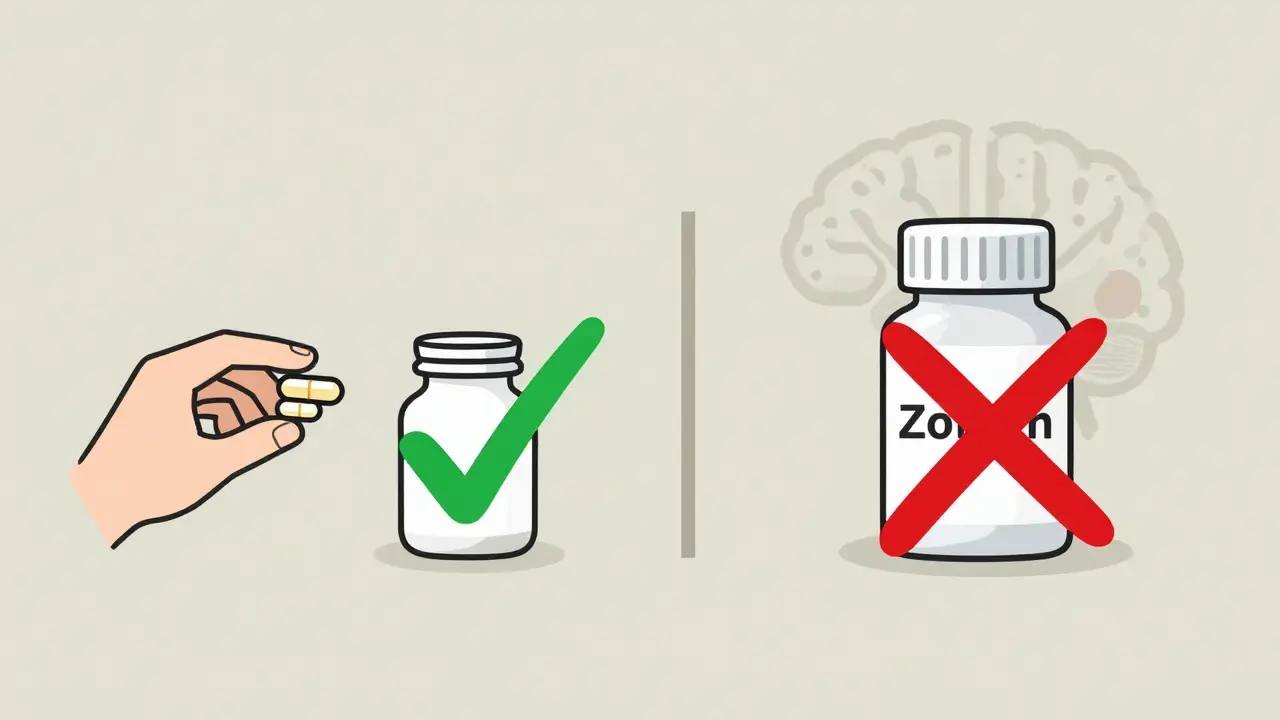
The Risky Ones: What to Avoid or Reserve for Last Resort
Ondansetron (Zofran) is popular. It’s strong. It works fast. And it’s often prescribed off-label for severe nausea. But here’s what doctors don’t always tell you: a 2012 NIH study found a 2.37-fold increase in cerebral palsy risk among babies exposed to ondansetron in the first trimester. That’s not a small number. It’s not a theory. It’s a statistical signal that’s repeated in multiple studies. While the absolute risk is still low, the relative risk is high enough that experts now warn against using it unless absolutely necessary.
Then there’s ondansetron’s side effect profile: headaches in 42% of users, dizziness in 37%, constipation in 29%. On Drugs.com, 32% of reviews flagged these as severe enough to stop taking it. For a condition that usually improves by week 14, why risk it?
Proton pump inhibitors (PPIs) like omeprazole are often used for heartburn, but they’re not harmless in early pregnancy. The same NIH study found a 4.36-fold increase in hypospadias - a condition where the urethra doesn’t form properly - when PPIs were taken in the first trimester. That’s a huge jump. If you’re using PPIs for acid reflux, talk to your provider about switching to antacids with calcium carbonate instead. Those actually lower the risk of cleft lip/palate.
Corticosteroids? They work for extreme cases of hyperemesis gravidarum - but they carry a 3.4-fold higher risk of cleft lip or palate. These are reserved for hospital settings, and only when every other option has failed.
What About Acupressure and Other Alternatives?
Wristbands, essential oils, acupuncture - they’re everywhere. But the science doesn’t back them up. The 2023 Frontiers meta-analysis showed acupressure bands had the same effect as placebo. No benefit. No harm. But no real help either. If you feel better using them, fine. But don’t rely on them if you’re struggling to keep fluids down.
Same goes for peppermint tea, lemon water, or ginger candy. They might soothe you, but they won’t stop vomiting. They’re comfort measures, not treatments. Use them alongside proven options, not instead of them.
When to Start Medication - Don’t Wait
Many people wait until they’re dehydrated, losing weight, or can’t leave the house before seeking help. That’s a mistake. The American College of Obstetricians and Gynecologists (ACOG) says early treatment prevents hospitalization. If you’re nauseous every day and can’t eat without gagging, that’s enough to start treatment. You don’t need to be vomiting blood or fainting.
Most women - 89% - get control of symptoms with first-line options. Only 10-11% need stronger meds. Waiting too long doesn’t make you stronger. It makes recovery harder.
Managing Side Effects: Practical Tips
Drowsiness from doxylamine? Take it at night. Don’t drive or operate machinery after taking it. Constipation from prenatal vitamins? Switch to an iron-free version in the first trimester. Iron worsens nausea and constipation - two problems that feed each other. Calcium-based antacids help with both heartburn and nausea, and they’re safer than PPIs.
Keep a symptom journal. Note what you ate, what you took, and how you felt. Patterns emerge. Maybe ginger helps after breakfast but not lunch. Maybe doxylamine works better if you take it at 8 p.m. instead of 10. Small tweaks make a big difference.
What’s Changing in 2025?
ACOG is updating its guidelines this year, likely to downgrade ondansetron to a last-resort option. The FDA is also tightening requirements for new antiemetics studied in pregnancy, demanding more data on long-term outcomes. Meanwhile, ginger remains the most recommended complementary therapy - 92% of obstetricians now suggest it as a first step.
And here’s something hopeful: the more women speak up about their symptoms, the more providers listen. Nausea isn’t just ‘normal’ - it’s a medical issue that deserves care. You’re not being dramatic. You’re not weak. You’re pregnant, and your body is under stress. You deserve relief - safely.
Bottom Line: Your Treatment Roadmap
Start here:
- Try ginger (250 mg four times a day)
- Add pyridoxine (25 mg three times a day)
- If still struggling, add doxylamine (25 mg at bedtime)
- If that doesn’t work, try an antihistamine like meclizine or dimenhydrinate
- Only consider ondansetron if you’re losing weight, dehydrated, or hospitalized - and only after discussing risks with your provider
- Avoid PPIs and corticosteroids unless absolutely necessary
Most women find relief within a week. And by week 16, for most, it’s gone. But until then - you don’t have to suffer. There are safe choices. You just need to know which ones to pick.
Is it safe to take ginger during pregnancy for nausea?
Yes, ginger is considered safe and effective for pregnancy nausea. Studies show 250 mg taken four times daily reduces nausea by over 50% with no increased risk of birth defects. It’s recommended by ACOG as a first-line option. Some people find the taste strong, but capsules are widely available and well-tolerated.
Can I take Zofran (ondansetron) while pregnant?
Zofran is not recommended as a first- or second-line treatment. Studies link it to a 2.37-fold increased risk of cerebral palsy in babies exposed during the first trimester. It’s only considered if you’re severely dehydrated, losing weight, or hospitalized - and even then, only after safer options have failed. Side effects like headaches and constipation are common.
Is Diclegis better than taking B6 and Unisom separately?
No - Diclegis is just a delayed-release version of pyridoxine and doxylamine, the same ingredients found in over-the-counter B6 and Unisom. Taking them separately is equally effective and much cheaper. Diclegis costs over $300 for a 30-day supply; the same dose in OTC form costs less than $15. The only advantage is convenience - not safety or effectiveness.
Are antacids safe during pregnancy?
Yes, antacids with calcium carbonate (like Tums) are not only safe - they’re beneficial. They reduce heartburn and nausea, and studies show they’re linked to a lower risk of cleft lip/palate. Avoid antacids with aluminum or magnesium in large doses. Stick to calcium-based ones, and use them as needed.
When should I call my doctor about morning sickness?
Call your provider if you can’t keep any food or fluids down for 24 hours, lose more than 5% of your pre-pregnancy weight, feel dizzy or faint, notice dark urine or infrequent urination, or have vomit with blood in it. These are signs of dehydration or hyperemesis gravidarum, which need medical treatment. Don’t wait until you’re hospitalized - early help prevents complications.
Do prenatal vitamins make nausea worse?
Yes - especially those with iron. Iron can worsen nausea and constipation. If your prenatal vitamin is making you feel worse, ask your provider about switching to an iron-free version during the first trimester. You can start iron supplements later, when nausea improves. Some women find chewable or liquid prenatal vitamins easier to tolerate.
If you’re struggling with nausea right now, know this: you’re not alone, and you don’t have to power through it. The right treatment exists. Start simple. Stay safe. And don’t hesitate to ask for help - your health matters just as much as your baby’s.

Diana Alime
December 24, 2025 AT 11:36