When someone is diagnosed with multiple sclerosis, the real fear isn’t just the relapses-it’s the quiet, steady decline that follows. You might feel fine one day, then wake up with numbness, blurred vision, or trouble walking. These flare-ups come and go, but over time, the damage doesn’t fully heal. That’s not just inflammation. It’s something deeper: your nerves are slowly falling apart.
What Happens Inside the Nervous System in MS?
Multiple sclerosis isn’t just about the immune system attacking the brain and spinal cord. It’s about what happens after the attack. The immune system targets the myelin sheath-the fatty coating that wraps around nerve fibers like insulation on a wire. When myelin gets stripped away, electrical signals slow down or stop. That’s why you get symptoms like weakness, tingling, or balance problems.
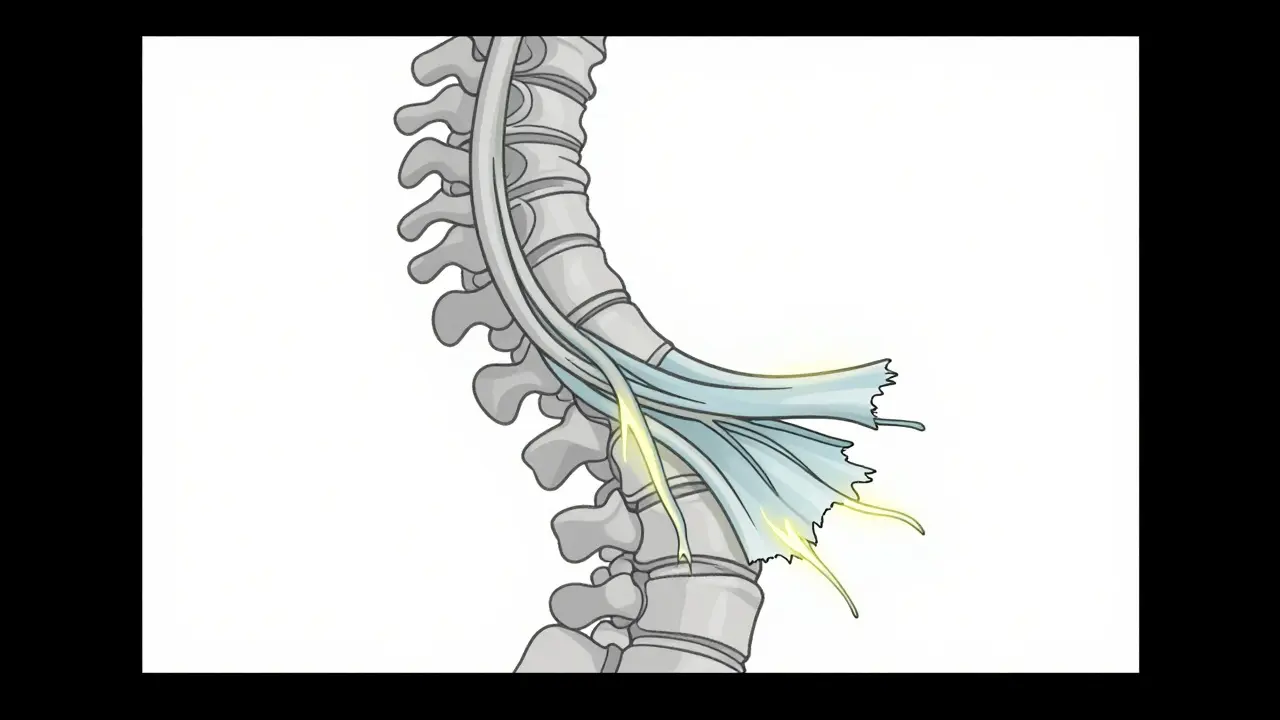
But here’s the critical part: the nerve fibers themselves-called axons-start breaking down too. And once an axon dies, it doesn’t grow back. That’s why many people with MS eventually lose mobility, vision, or bladder control even when their flare-ups stop. This isn’t just a relapsing disease. It becomes a degenerative one.
Studies show that about 40% of people with relapsing-remitting MS (RRMS) will shift into secondary progressive MS (SPMS) within 10 to 15 years. In SPMS, the damage isn’t driven by new inflammatory lesions on MRI scans. Instead, it’s the slow, hidden loss of axons and neurons. The brain’s ability to compensate fades. The nerves can’t repair themselves. And the damage accumulates silently.
Why Inflammation Isn’t the Whole Story
For years, doctors treated MS like an autoimmune flare-up-something you could calm down with steroids or immune-suppressing drugs. And for a while, it worked. Newer disease-modifying therapies (DMTs) can cut relapse rates by 30% to 50% in RRMS. But they don’t stop progression.
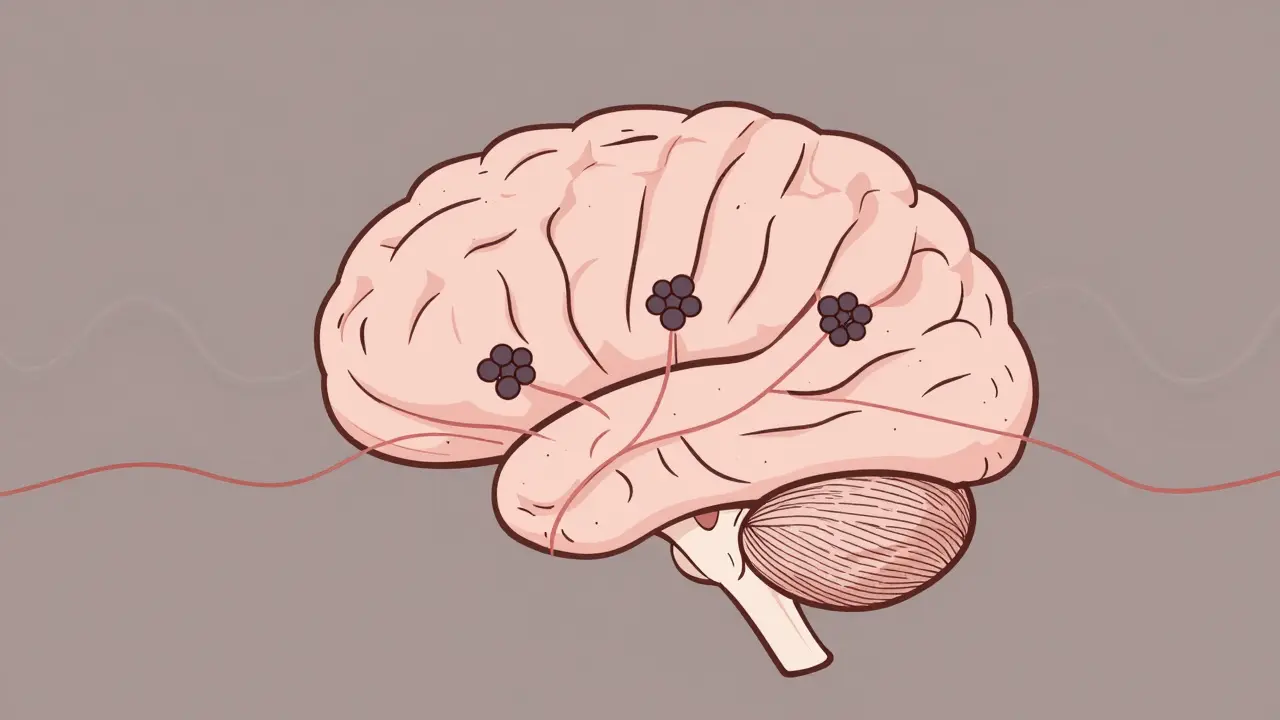
Why? Because once the disease moves into its progressive phase, the problem shifts. Inflammation doesn’t disappear, but it changes. Instead of immune cells flooding in from the bloodstream, immune activity happens inside the brain itself. B cells cluster around the meninges-the protective layers around the brain-and create what look like tiny lymph node-like structures. These areas release chemicals that poison nearby nerve fibers.
And here’s the grim reality: current DMTs don’t reach these areas well. Drugs that work on blood-borne immune cells can’t cross the blood-brain barrier effectively in later stages. So even if you’re taking your medication every day, the damage inside your brain may still be ticking forward.
The Real Culprit: Axonal Degeneration
The biggest reason MS leads to permanent disability isn’t the plaques you see on an MRI. It’s what’s happening to the axons. In chronic MS lesions, half of the demyelinated axons show signs of breakdown: swollen, fragmented, missing mitochondria-the energy factories that keep nerves alive.
Without myelin, axons have to work harder. They pump more sodium in to keep signals moving. But that uses up energy. Over time, the mitochondria burn out. The sodium pumps fail. The axons starve. And then they die.
Research shows that axonal loss correlates directly with disability. The more axons you lose, the worse your walking speed, hand function, and cognition become. Brain atrophy-especially in the gray matter-is a better predictor of long-term decline than the number of new lesions. That’s why doctors now track brain volume changes over time, not just new spots on scans.
Why Current Treatments Fall Short
There are 21 FDA-approved disease-modifying therapies for MS. All of them target inflammation. None of them directly protect axons or repair myelin.
Drugs like interferons, glatiramer acetate, fingolimod, and ocrelizumab reduce relapses. Some slow the formation of new lesions. But in SPMS and PPMS, where inflammation is minimal, these drugs show little to no benefit. That’s why many patients with progressive MS are told, “There’s nothing more we can do.”
It’s not that the science is stuck. It’s that the tools we have were designed for the wrong phase of the disease. We’ve spent decades treating MS like a fire. But what we need now are tools to rebuild the house after the fire’s out.
The Future: Protecting Nerves, Not Just Fighting Inflammation
Scientists are now chasing therapies that target the real drivers of progression:
- Neuroprotection: Drugs that block sodium channels on axons to reduce energy demand. Early trials with drugs like riluzole and siponimod show promise in slowing disability.
- Mitochondrial support: Since nerve cells starve without energy, researchers are testing compounds like biotin and idebenone to boost mitochondrial function.
- Remyelination: Trials are underway with drugs like opicinumab and clemastine, which aim to wake up the brain’s own stem cells to rebuild myelin.
- Targeting B cells in the brain: New drugs are being designed to cross the blood-brain barrier and shut down meningeal inflammation directly.
As of late 2023, there are 17 active Phase II and III trials focused on progressive MS. For the first time, researchers are measuring outcomes not just by relapses, but by walking speed, hand dexterity, and brain volume loss.
What You Can Do Now
Even if you’re on a DMT, there are steps you can take to protect your nervous system:
- Keep vitamin D levels high: Low vitamin D is linked to faster progression. Aim for blood levels above 75 nmol/L-many neurologists recommend 100-150 nmol/L.
- Stop smoking: Smokers with MS progress twice as fast. Quitting can slow disability by up to 50%.
- Exercise regularly: Aerobic activity increases brain-derived neurotrophic factor (BDNF), which helps nerves survive. Even 30 minutes of walking or swimming five times a week makes a difference.
- Manage stress: Chronic stress raises cortisol, which may worsen inflammation and reduce repair mechanisms.
- Track your function: Use tools like the MSFC (Multiple Sclerosis Functional Composite) to monitor walking, hand strength, and cognition-not just EDSS scores. You’ll catch decline earlier.
It’s Not Hopeless
For decades, MS was seen as a one-way slide into disability. But that view is changing. We now know that progression isn’t inevitable. It’s driven by specific biological processes-and those processes can be targeted.
The next five years will bring the first true neuroprotective drugs for MS. They won’t cure it. But they might stop the slow erosion of your nerves. That’s not a cure. But for someone who’s watched their body fade over years, it’s everything.
What matters now isn’t just controlling relapses. It’s protecting what’s left. And that’s a fight worth fighting.
Can disease-modifying therapies stop MS progression?
Current disease-modifying therapies (DMTs) reduce relapses and new lesions in relapsing-remitting MS by 30-50%, but they don’t stop progression in secondary or primary progressive MS. Once axonal degeneration takes over, inflammation-targeting drugs have little effect. New neuroprotective therapies in clinical trials aim to address this gap.
Why do some people with MS get worse even without new lesions?
Progressive MS is driven by damage inside the brain and spinal cord that isn’t visible on standard MRI scans. Axons degenerate over time due to chronic demyelination, mitochondrial failure, and low-grade inflammation from B cells in the meninges. This process continues even when no new lesions form, leading to steady decline.
Is brain atrophy a sign of MS progression?
Yes. Brain atrophy-especially gray matter loss-is one of the strongest predictors of long-term disability in MS. Studies show that people with faster brain volume loss over 2-4 years are more likely to experience worsening mobility, cognition, and function. MRI scans measuring brain volume are now used alongside clinical tests to track progression.
Can lifestyle changes slow MS progression?
Absolutely. Quitting smoking can cut progression risk by up to 50%. Maintaining vitamin D levels above 75 nmol/L, exercising regularly, and managing stress reduce inflammation and support nerve health. These aren’t cures, but they’re proven ways to protect your nervous system and delay disability.
Are there any new drugs for progressive MS?
Yes. As of 2023, there are 17 active clinical trials testing drugs that target neurodegeneration in progressive MS. These include sodium channel blockers, mitochondrial boosters, and remyelination agents. Siponimod is the first DMT approved for SPMS that shows modest slowing of disability progression, likely by acting inside the central nervous system.
Lana Kabulova
January 21, 2026 AT 12:47