When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your blood’s acid levels in check. That’s when metabolic acidosis creeps in. It’s not a flashy disease, but it’s one of the most common, underdiagnosed, and treatable problems in people with chronic kidney disease (CKD). And if left alone, it doesn’t just make you feel tired-it speeds up your kidney decline, eats away at your muscles, and weakens your bones.
What Exactly Is Metabolic Acidosis?
Metabolic acidosis happens when your blood gets too acidic. Normal blood pH is between 7.35 and 7.45. When it drops below 7.35 and your serum bicarbonate falls under 22 mEq/L, you’ve crossed into metabolic acidosis. In healthy people, the kidneys balance this by getting rid of acid and making more bicarbonate. But in CKD, that system breaks down. By stage 3, about 15% of patients already have it. By stage 5? Nearly half do.This isn’t just a lab number. It’s a silent thief. Every day your blood stays too acidic, your body starts pulling calcium from your bones to neutralize it. Your muscles break down because your body uses them as fuel to fight the acid. Your heart works harder. And your kidneys? They keep deteriorating faster.
Why Bicarbonate Is the Go-To Treatment
The most straightforward fix? Give back what the kidneys can’t make-bicarbonate. Sodium bicarbonate tablets (650mg each, delivering about 7.6 mEq) are the most common treatment. Some people use baking soda powder-one teaspoon gives you 50 mEq. It’s cheap, widely available, and works.A major 3-year trial with 740 CKD patients showed that those taking sodium bicarbonate slowed their eGFR decline by nearly 6 mL/min/1.73m² compared to those who didn’t. That’s not just a number-it means delaying dialysis by years for many. The KDIGO guidelines recommend starting treatment when bicarbonate drops below 22 mEq/L. The target? Keep it between 23 and 29 mEq/L.
But here’s the catch: sodium bicarbonate comes with sodium. A single 500mg tablet has 610mg of sodium. For someone with high blood pressure or heart failure, that’s dangerous. It can cause fluid retention, swelling, and hospitalizations. One study found that CKD patients on sodium bicarbonate had a 32% higher chance of being admitted for heart failure than those on calcium citrate.
Alternatives to Sodium Bicarbonate
Not everyone can tolerate sodium bicarbonate. That’s where other options come in.- Sodium citrate (Shohl’s solution): 1 mEq per mL. Less sodium than baking soda, but still not ideal for heart failure patients.
- Potassium citrate: Great for kidney stones and low potassium-but risky in CKD. About 18% of patients on it develop dangerous high potassium levels (hyperkalemia). Avoid if your potassium is above 4.5 mEq/L.
- Calcium citrate: Gives you bicarbonate without extra sodium. But it adds calcium. Long-term use can raise your blood calcium and increase kidney stone risk by 27%.
One patient in Cleveland shared on a kidney forum: "I switched from sodium bicarbonate to calcium citrate. Now I take six pills a day. Still get leg cramps. But at least my blood pressure is stable."
Diet Can Help-If You Stick With It
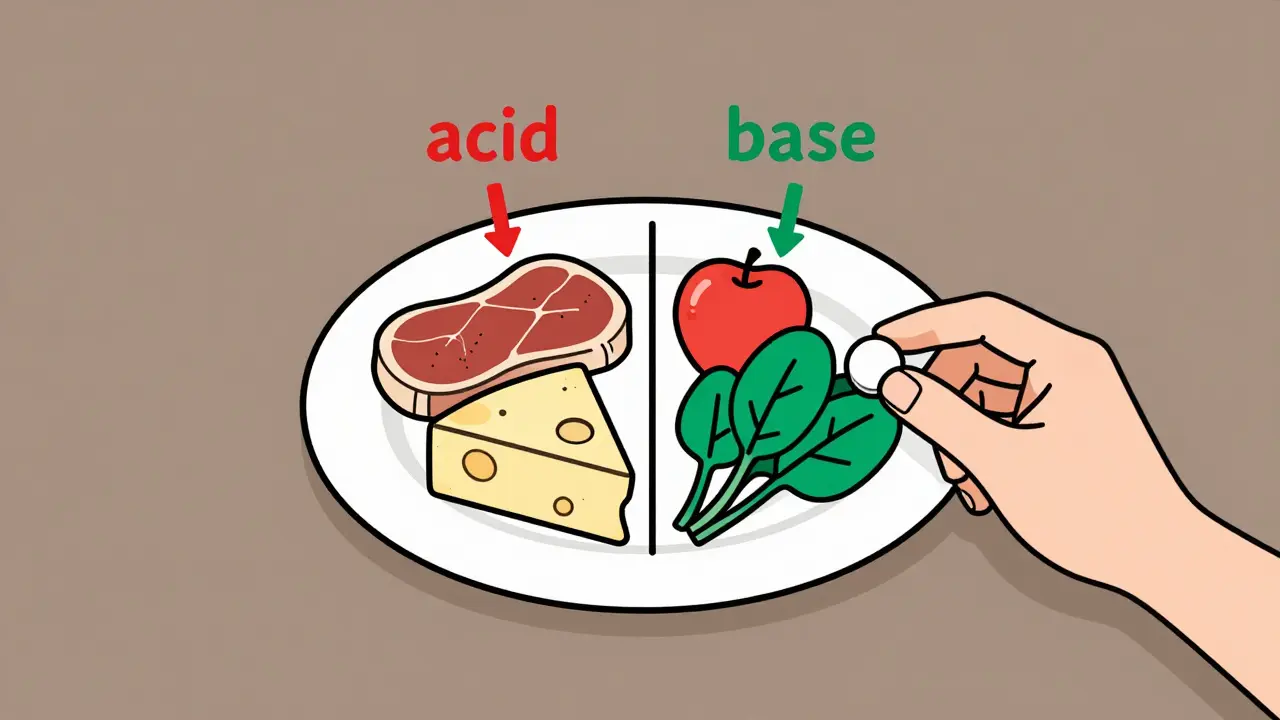
Food plays a huge role. Some foods are acid factories: meat, cheese, processed grains. Others are natural buffers: fruits, vegetables, legumes.Meat adds +9.5 mEq of acid per 100g. Cheese? +8.0. Apples? -2.2. Spinach? -2.8. The goal is to flip your plate. Make half your meals fruits and vegetables. That can cut your daily acid load by 40-60 mEq.
One study showed that patients who followed a plant-heavy diet for six months saw their bicarbonate rise by 3.5 mEq/L-without any pills. But here’s the problem: adherence. Most people struggle. The taste of baking soda in water is awful. One Reddit user said they had to mix it with orange juice, which added sugar they shouldn’t be consuming. Another said they couldn’t handle the bloating and nausea.
A 2022 survey of 457 CKD patients found that 68% found their medication regimen too heavy (average 4.2 pills a day), 41% hated the taste, and 29% had GI side effects. Diet changes require education, time, and support. Only 35% of patients ever hit the target of a neutral or negative Potential Renal Acid Load (PRAL).
The New Hope That Didn’t Pan Out
For years, there was buzz around veverimer-a non-absorbed polymer that traps acid in the gut. No sodium. No potassium. No calcium. Just acid removal. Phase 2 trials looked great: bicarbonate jumped by 4.3 mEq/L in 12 weeks.Then came phase 3. The results? Not good enough. The difference between veverimer and placebo was 2.07 mEq/L-statistically insignificant. The FDA didn’t approve it. Tricida Inc. plans to resubmit in 2024 with new data, but for now, it’s not an option.
Meanwhile, a new citrate-free alkali supplement called TRC001 showed promise at the 2023 ASN meeting. It raised bicarbonate by 4.1 mEq/L in 12 weeks-with half the stomach issues of sodium citrate. It’s still in trials, but it’s one to watch.
Who Gets Treated-and Who Doesn’t
Here’s the uncomfortable truth: even though we know metabolic acidosis harms kidneys, most people with it don’t get treated. A 2023 analysis found only 43% of eligible CKD patients receive alkali therapy. The gap is worse in rural areas (35% treated) than urban (49%). Black patients are less likely to get it than white patients (38% vs. 47%).Why? Lack of awareness. Lack of monitoring. Lack of time in busy clinics. Many nephrologists check bicarbonate every 3-6 months, but if you’re not flagged early, you slip through the cracks.
The National Kidney Foundation says 78% of nephrologists use PRAL scores to assess dietary acid load. But only 35% of patients ever reach a neutral PRAL. That’s a huge gap between knowing what to do and actually doing it.
What You Should Do Right Now
If you have CKD and haven’t had your bicarbonate checked in the last six months, ask for it. It’s a simple blood test. If it’s under 22 mEq/L, talk to your doctor about treatment.Start here:
- Get your serum bicarbonate level tested.
- If it’s below 22 mEq/L, ask if you’re a candidate for alkali therapy.
- If you have high blood pressure or heart failure, discuss calcium citrate or dietary changes first.
- Ask for a referral to a renal dietitian. Learn which foods help and which hurt.
- Track your symptoms: fatigue, muscle cramps, swelling, or shortness of breath.
Don’t wait for your kidneys to fail before you act. Correcting metabolic acidosis isn’t about feeling better today-it’s about keeping your kidneys working longer. Studies show that keeping bicarbonate above 22 mEq/L cuts your risk of needing dialysis or losing half your kidney function by 23%.
What’s Coming Next
The KDIGO guidelines are updating in 2024. The new draft suggests a broader target: 22-29 mEq/L. Why? Because even 22 mEq/L seems to protect kidneys. For elderly patients with frailty or malnutrition, they’re now suggesting 22-24 mEq/L. For those with heart failure? 24-26 mEq/L.The COMET-CKD trial is testing high-dose vs. low-dose sodium bicarbonate. Results come in late 2025. That could change dosing standards.
And if TRC001 or another new agent gets approved, we might finally have a treatment that works without the sodium, potassium, or calcium risks.
For now, the tools we have work-if we use them. Metabolic acidosis isn’t inevitable in CKD. It’s a treatable condition. And treating it isn’t just about chemistry. It’s about keeping people out of the hospital, off dialysis, and living longer with better quality of life.
How do I know if I have metabolic acidosis?
You won’t feel it at first. It’s usually found through a routine blood test that checks your serum bicarbonate level. If it’s below 22 mEq/L and you have CKD, you likely have metabolic acidosis. Symptoms like fatigue, muscle weakness, or rapid breathing may appear later, but many people have no symptoms until the condition is advanced.
Can I treat metabolic acidosis with just diet?
Diet can help, but it’s rarely enough on its own if your bicarbonate is below 20 mEq/L. Eating more fruits and vegetables and cutting back on meat and cheese can reduce acid load by 40-60 mEq per day. Some patients see a 3-4 mEq/L rise in bicarbonate after six months. But for most with moderate to severe acidosis, you’ll still need oral alkali therapy like sodium bicarbonate or calcium citrate.
Is baking soda safe for CKD patients?
Baking soda (sodium bicarbonate) is effective, but not safe for everyone. If you have high blood pressure, heart failure, or swelling, it can make things worse due to its high sodium content. One teaspoon contains 50 mEq of bicarbonate and over 1,200mg of sodium. Only use it under medical supervision, and never as a DIY remedy without monitoring your blood pressure and fluid status.
Why isn’t potassium citrate recommended for CKD?
Potassium citrate can raise your potassium levels, which is dangerous in CKD. About 45% of stage 3b-5 patients already have elevated potassium. Adding potassium citrate can push it into the dangerous range (>5.0 mEq/L), leading to heart rhythm problems. It’s only used if you’re low in potassium and your doctor carefully monitors you.
How often should my bicarbonate be checked?
If you’re stable and not on treatment, check every 6 months. If you’re starting or adjusting alkali therapy, check monthly until levels stabilize. Once you’re at target (23-29 mEq/L), you can go back to every 3-6 months. Regular monitoring is the only way to catch changes before they harm your kidneys.
What’s the best long-term strategy for managing metabolic acidosis in CKD?
A combination approach works best: start with diet (5-9 servings of fruits and vegetables daily), add oral alkali if needed, choose the form that fits your health profile (calcium citrate if you have heart issues, sodium bicarbonate if you don’t), and monitor your levels regularly. Work with a renal dietitian. Avoid potassium citrate unless you’re low in potassium. And don’t ignore the symptoms-fatigue and muscle loss aren’t just "part of aging." They could be signs your blood is too acidic.

Josh Potter
December 16, 2025 AT 03:38