When hot flashes hit at 3 a.m. for the 15th time this week, and sleep, mood, and energy vanish like smoke, it’s hard not to wonder: is hormone therapy worth it? For millions of women, the answer isn’t yes or no-it’s maybe, but only if it’s right for you. Menopause isn’t a disease. But for many, the symptoms are debilitating. And hormone therapy (MHT), once vilified, is now being reevaluated with far more nuance than before.
What Hormone Therapy Actually Does
Menopause hormone therapy (MHT) replaces the estrogen and sometimes progesterone your body stops making after your last period. It’s not a fountain of youth. It doesn’t reverse aging. But it does something powerful: it shuts down the worst of menopause’s physical chaos. For women with severe hot flashes, night sweats, or vaginal dryness, MHT can cut symptoms by 75% or more. That’s not a guess-it’s from large, long-term studies like the Women’s Health Initiative.Estrogen alone works for women who’ve had a hysterectomy. For those with a uterus, you need progesterone too-otherwise, the lining of the uterus thickens, raising the risk of endometrial cancer. That’s why combination therapy is standard unless you’ve had your uterus removed.
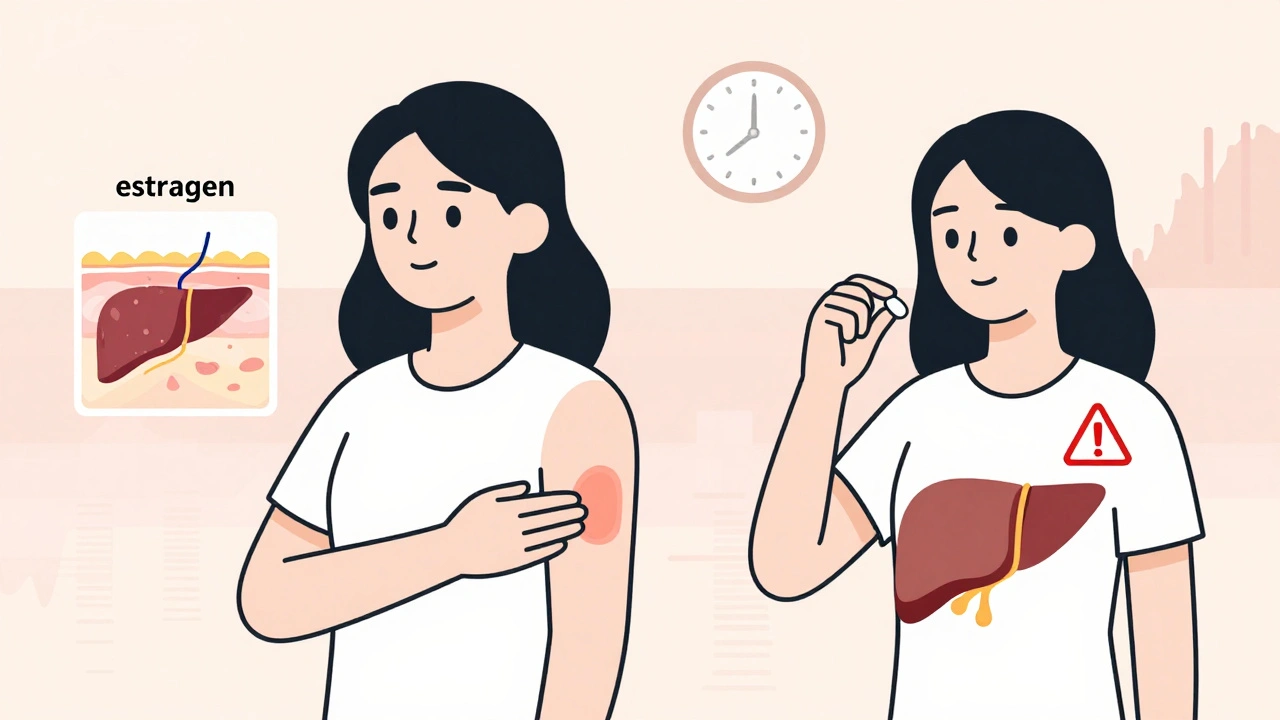
The forms matter too. Pills are common, but patches, gels, sprays, and vaginal rings deliver estrogen directly through the skin or mucous membranes. That’s important because when estrogen goes through the liver (as it does with pills), it increases clotting factors. Transdermal estrogen avoids that. Studies show transdermal routes lower the risk of blood clots and strokes by up to 30% compared to oral pills.
The Real Risks-Not the Scare Stories
The big fear around MHT? Breast cancer. And yes, it’s real-but not as simple as “hormones cause cancer.” The risk depends on what you take, how long, and when you start.For women taking estrogen plus progestogen (combination therapy), studies show about 29 extra cases of breast cancer per 10,000 women per year. That sounds alarming, but put it in context: the baseline risk of breast cancer for a 55-year-old woman is about 23 cases per 10,000 per year. So combination therapy adds roughly 1 extra case per 350 women each year. Estrogen-only therapy (for women without a uterus) shows no significant increase in breast cancer risk-just 9 extra cases per 10,000 women per year.
Timing is everything. Starting MHT before age 60 or within 10 years of your last period appears much safer than starting later. The “timing hypothesis” is now widely accepted: your body responds better to hormones when it’s still close to its natural hormonal state. Starting after 60, especially if you have high blood pressure or other heart risks, increases your chance of stroke and heart attack.
Other risks? Blood clots are more common with oral estrogen-especially in women who are overweight, smoke, or have a history of clots. The risk is still low: about 3 in 1,000 women per year on oral therapy, compared to 1.3 on patches. Gallbladder disease is slightly more likely with pills. And yes, MHT can cause bloating, breast tenderness, or mood swings-especially in the first few months. Most of these fade with dose adjustments.
What Hormone Therapy Won’t Do
Let’s be clear: MHT is not a magic shield against aging. It won’t prevent dementia. It won’t protect your heart if you start it late. The Women’s Health Initiative found that women who began MHT after age 65 had a higher risk of dementia-not because hormones cause it, but because their brains may have already begun changing.It also doesn’t replace exercise, calcium, or vitamin D for bone health. While MHT does preserve bone density and cuts fracture risk by 30-40%, it’s not the only tool. Weight-bearing exercise, protein intake, and fall prevention are just as important.
And no, MHT won’t fix sleep if your insomnia is caused by stress, anxiety, or sleep apnea. It might help if hot flashes are waking you up-but if you’re lying awake worrying about your kids, your job, or your finances, hormones won’t fix that.
Alternatives That Actually Work
Not everyone wants hormones. And that’s okay. There are other options, though they’re not as strong.SSRIs like paroxetine (Brisdelle) are FDA-approved for hot flashes. They reduce symptoms by about 50-60%. Gabapentin helps too, but about 1 in 4 people get dizzy or drowsy. Neither is as effective as estrogen.
Plant-based options like soy, flaxseed, or black cohosh? The science is messy. A Cochrane Review found they reduce hot flashes by less than half a day per week-barely better than a placebo. They’re safe for most, but don’t expect miracles.
Lifestyle changes? Yes. Cooling your bedroom, wearing layers, avoiding alcohol and spicy food, and practicing paced breathing can help. One study showed women who did daily breathing exercises cut hot flashes by 40% in 8 weeks. Not as much as hormones-but no pills, no risks.
Who Should Avoid It
Some women should not use MHT at all. That includes:- Women with a history of breast cancer (especially estrogen-receptor positive)
- Those who’ve had a blood clot, stroke, or heart attack
- Women with undiagnosed vaginal bleeding
- Anyone with active liver disease
- Those with a history of estrogen-sensitive cancers like ovarian or uterine cancer
If you have a strong family history of breast cancer or clotting disorders, talk to your doctor about genetic testing. Some women carry mutations like BRCA1 or Factor V Leiden that change the risk calculus.
How to Get Started-Safely
If you’re considering MHT, don’t just ask your GP for a prescription. Ask for a plan.- Track your symptoms for a month. Use a simple app or notebook. How many hot flashes? How bad is sleep? Any mood changes?
- Get your blood pressure checked. High blood pressure raises stroke risk with oral estrogen.
- Discuss your personal and family history. Do you have a history of clots, cancer, or heart disease?
- Start low. The lowest effective dose is best. For most, that’s 0.5 mg of oral estradiol or a 0.025 mg patch.
- Choose transdermal if you can. Patches or gels are safer for your heart and blood.
- Use progesterone only if you have a uterus. Micronized progesterone (Prometrium) is better tolerated than synthetic progestins like medroxyprogesterone.
- Revisit your plan every 6-12 months. Can you lower the dose? Can you stop?
Most women who start MHT for symptoms don’t need to stay on it forever. Many taper off after 2-5 years. Your body adapts. Your symptoms often fade. The goal isn’t lifelong use-it’s relief during the toughest years.
What’s Changing in 2025
The conversation around MHT is shifting fast. In July 2025, the FDA opened a public docket asking for more data on how timing, dosage, and delivery method affect risk. A landmark study presented at The Menopause Society’s annual meeting analyzed 120 million patient records and found that starting estrogen during perimenopause-before your periods fully stop-cut heart disease risk by 18% compared to starting after menopause.Experts are now talking about a “window of opportunity”-the 10-year span after your last period. Start MHT within that window, and benefits outweigh risks for most healthy women. Start later, and the risks climb.
Soon, we may see personalized hormone therapy based on genetics. Researchers are already testing how women metabolize estrogen. Some break it down quickly. Others hold onto it longer. That could mean custom dosing based on your DNA-not a one-size-fits-all pill.
Real Stories, Real Choices
One woman in Wellington started a 0.05 mg estradiol patch at 52 after years of 20 hot flashes a day. Within 10 days, she was down to two. She slept through the night for the first time in three years. She’s been on it for five years. Her bone density is stable. She checks in with her doctor every year.Another woman, 58, took oral Prempro for three years after her husband died. She felt better at first. Then she had a small, non-invasive breast cancer. She stopped MHT immediately. She’s fine now-but she says, “I wish I’d known how much timing mattered.”
And a third woman, 56, chose no hormones. She uses cooling sheets, walks daily, and takes magnesium. Her hot flashes are still there, but she’s okay with that. “I’d rather be a little uncomfortable than take a pill that might hurt me later,” she says.
There’s no right answer for everyone. But there is a right answer for you. And it starts with knowing your numbers, your history, and your priorities.
Is hormone therapy safe for women under 60?
Yes-for most healthy women under 60 or within 10 years of menopause, the benefits of hormone therapy for symptom relief and bone protection outweigh the risks. The key is using the lowest effective dose, preferably transdermal, and avoiding long-term use unless necessary. Studies show women in this group have a lower risk of heart disease and fractures without a significant increase in breast cancer or stroke.
Does hormone therapy cause weight gain?
Not directly. Weight gain during menopause is usually due to aging, slower metabolism, and reduced muscle mass-not hormones. Some women retain water temporarily when starting MHT, but this usually goes away. In fact, better sleep and energy from reduced hot flashes can make it easier to stay active and manage weight.
Can I use hormone therapy if I’ve had breast cancer?
Generally, no. Hormone therapy is not recommended for women with a history of estrogen-receptor positive breast cancer. Even low-dose or topical estrogen can stimulate cancer cells. Some women with very low-risk, non-hormone-sensitive cancers may be considered on a case-by-case basis, but only under strict supervision by an oncologist and menopause specialist.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women take MHT for 2-5 years to get through the worst symptoms. If symptoms return after stopping, you can restart at a lower dose. For women with severe bone loss or early menopause, longer use may be needed-but only with regular monitoring. The goal is always the shortest duration possible for the needed benefit.
Are natural or herbal remedies as good as hormone therapy?
No. While herbs like black cohosh or soy isoflavones are safe for many, they reduce hot flashes by only about 0.5 per day on average-barely better than a placebo. Hormone therapy reduces them by 75% or more. If your symptoms are mild, natural options might help. If they’re severe, MHT is the only treatment with strong, proven results.
What’s the difference between bioidentical and synthetic hormones?
Bioidentical hormones (like estradiol and micronized progesterone) have the same chemical structure as what your body makes. Synthetic hormones (like medroxyprogesterone acetate) are altered in a lab. Bioidentical forms are preferred because they’re better tolerated and linked to lower risks of blood clots and breast cancer. Compounded “bioidentical” hormones sold in specialty pharmacies are not FDA-approved and lack safety data-stick to regulated, pharmacy-dispensed versions.
If you’re unsure where to start, find a certified menopause practitioner. There are over 1,850 in the U.S. alone, and many offer virtual consultations. Don’t let outdated fears stop you from getting the care you need. Menopause is a medical transition-not a moral failing. You deserve relief, safety, and clarity.
parth pandya
December 3, 2025 AT 01:39