Medical Alert Bracelet Checklist
Find Out What You Need on Your Bracelet
Answer these questions to determine the critical information that should be on your medical alert bracelet. Your responses will help ensure emergency responders have the right information when you need it most.
Your Medical Alert Bracelet Recommendation
Every year, thousands of people end up in emergency rooms because of medication errors-many of which could have been avoided with a simple piece of jewelry on their wrist. A medical alert bracelet isn’t just a fashion accessory. For people taking blood thinners, managing diabetes, or living with severe drug allergies, it’s a lifeline. In a crisis, when you can’t speak, this bracelet speaks for you.
Why Medical Alert Bracelets Exist
The first medical alert bracelet was created in 1956 by the MedicAlert Foundation, designed to help doctors quickly identify life-threatening conditions. Today, over 4 million people worldwide wear them. Why? Because emergency responders are trained to check wrists and necks first. If you’re unconscious after a fall, having a seizure, or in shock from an allergic reaction, you won’t be able to tell the EMT that you’re on warfarin or allergic to penicillin. But your bracelet can.
According to the American College of Emergency Physicians (ACEP), nearly 37% of emergency room errors involve medications. That’s not a small number. It’s a system failure that affects real people. And the fix? Simple, cheap, and proven: wear a medical ID.
What Information Should Be on Your Bracelet?
Space is limited on a metal bracelet. You can’t fit your entire medication list. So what matters most?
- Drug allergies-especially penicillin, NSAIDs, aspirin, and sedatives. Penicillin allergies affect 10% of Americans. Anaphylaxis can kill in minutes. Your bracelet can stop a nurse from giving you the wrong antibiotic.
- Blood thinners-like warfarin, apixaban, or rivaroxaban. Over 2.9 million Americans take these. In trauma, giving a clotting agent to someone on a blood thinner can be deadly. Your bracelet tells them: “Don’t give this.”
- Diabetes type and insulin use-Type 1 vs. Type 2 changes emergency treatment. If you’re unconscious and your blood sugar is low, giving insulin instead of glucose could kill you. Your bracelet prevents that mistake.
- Chronic conditions-like epilepsy, heart failure, or kidney disease-can alter how drugs are metabolized. This info helps doctors avoid dangerous interactions.
According to the ID Band Company, 68% of their customers order bracelets with medication info. Of those, 42% list blood thinners. That’s not coincidence-it’s survival.
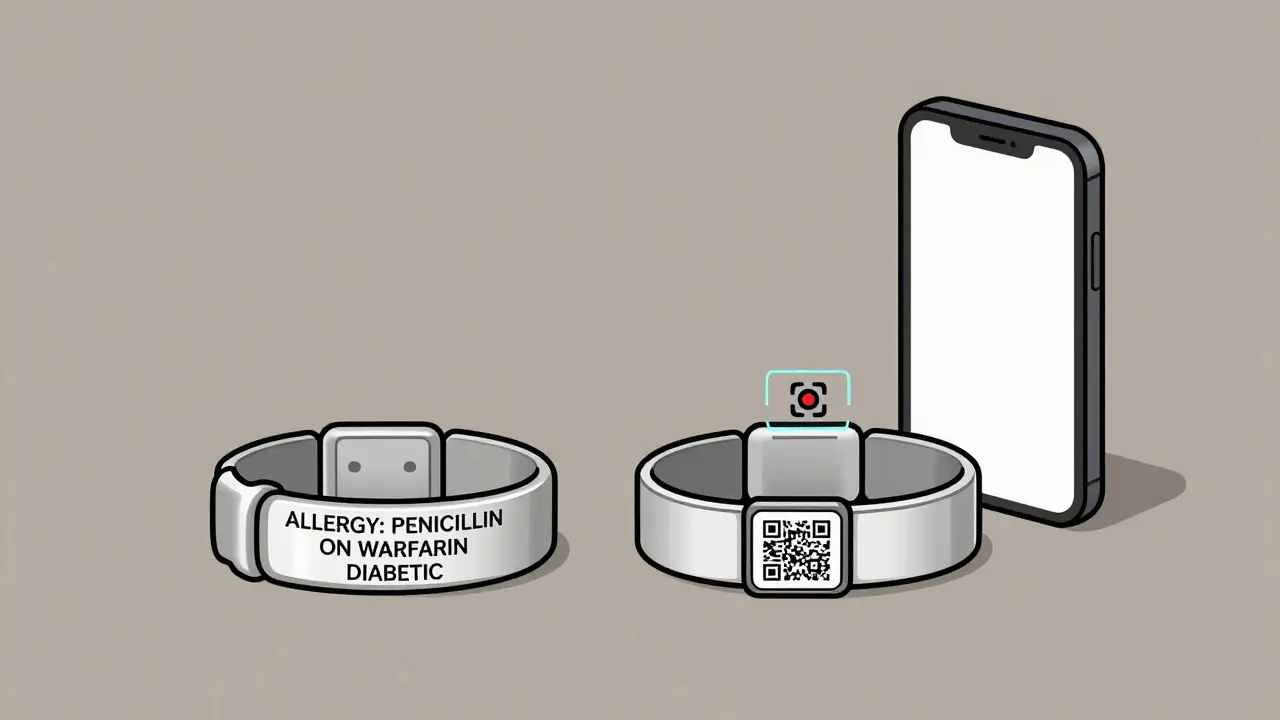
Traditional vs. QR Code Bracelets
There are two main types: engraved metal and digital QR code.
Traditional bracelets hold 3-5 critical items. They’re durable, waterproof, and don’t need batteries. But if you take five medications, have three allergies, and a pacemaker, you’re out of space. One user wrote: “My bracelet only says ‘ON BLOOD THINNERS’-but not which one. They still had to run tests.” That’s the risk.
QR code bracelets solve this. Scan the code with a phone, and you’re taken to a secure digital profile with your full medication list, dosages, doctor contacts, and even pharmacy info. MedicAlert’s SmartProfile system, launched in early 2024, syncs with pharmacy databases to auto-update your profile when your prescriptions change. No more forgetting to update your bracelet after your doctor switches your anticoagulant.
Traditional bracelets start at $49.99. QR code versions start at $69.99, with a $59.99 annual fee to maintain the digital profile. It’s not free-but neither is a preventable death.
Real Stories, Real Results
Reddit user AllergicAmy shared her story: “I was rushed to the ER for appendicitis. The nurse was about to give me penicillin. Then she saw my bracelet: ‘ANAPHYLACTIC TO PENICILLIN.’ She stopped. Later, she said, ‘You’d have been dead in five minutes.’”
Trustpilot reviews for MedicAlert show 4.7 out of 5 stars from over 1,200 users. Sixty-three percent say they bought it for drug safety. One man on warfarin said, “I had a fall last year. The paramedics checked my bracelet and knew not to give me ibuprofen. That saved my stomach from bleeding.”
But it’s not perfect. A 2023 Johns Hopkins audit found 19% of bracelets had outdated or incomplete info. If your bracelet says “warfarin” but you switched to apixaban six months ago, it’s worse than useless-it’s dangerous.
Keeping Your Info Current
Here’s the hard truth: 35% of users never update their bracelets after a medication change. That’s a gap between intention and action.
Fix it with systems:
- Set a calendar reminder every 3 months to review your meds and update your bracelet.
- Use a digital profile (like MedicAlert’s SmartProfile) that syncs with your pharmacy. When your doctor prescribes something new, the system auto-updates your bracelet’s online profile.
- Ask your pharmacist to print a checklist every time you pick up a new script. Tape it to your mirror. If it’s not on the bracelet, it’s not safe.
Medical Guardian’s 2025 system adds another layer: it pairs your bracelet with a personal alarm. If you fall, you press the button. Help comes. And while they’re coming, your bracelet tells them what to do. That combo improved emergency response effectiveness by 41% in NCOA’s 2024 study.
Who Needs One the Most?
You don’t need to be old or frail to benefit. High-risk groups include:
- People on blood thinners (41% of them wear IDs)
- Those with severe allergies (33% wear them)
- Diabetics on insulin (28% wear them)
- Anyone taking five or more medications
- People with cognitive issues or dementia
The FDA classifies these as Class I medical devices-meaning they’re low-risk but medically essential. And since the 2022 CARES Act, U.S. hospitals are required to check for them during emergency intake. Sixty-seven percent of hospitals now have formal protocols. That means your bracelet isn’t just helpful-it’s part of the system.
The Future: Smarter, Connected IDs
The next wave is integration. Epic Systems and Cerner, the two biggest electronic health record platforms, are building APIs that link your medical ID profile directly to your hospital chart. When your doctor changes your meds, your bracelet’s digital profile updates automatically.
The FDA’s 2023 Medical ID Modernization Initiative is pushing for standardized formatting. Soon, every bracelet will use the same language: “ALLERGY: PENICILLIN,” not “allergic to penicillin.” First responders won’t have to guess.
And AI is coming. Medical Guardian’s new system alerts you via phone if a new prescription could conflict with your emergency profile. It’s not science fiction-it’s here.
What to Do Now
If you take any medication that could cause harm in an emergency, get a medical alert bracelet. Don’t wait for a crisis.
- Identify your top 3 risks: allergies, blood thinners, or insulin dependence.
- Choose a trusted provider-MedicAlert, American Medical ID, or ID Band Company.
- Write only what matters: allergies first, then critical meds, then chronic conditions.
- Use a QR code if you have multiple meds or complex conditions.
- Set a quarterly reminder to review and update your info.
- Wear it every day-even when you’re at home. Seventy-three percent of emergencies happen away from home.
It’s not about fear. It’s about control. You can’t control when an accident happens. But you can control whether you’re prepared.
Do medical alert bracelets really work in emergencies?
Yes. First responders are trained to check for them, and they use the info in 89% of cases where the bracelet is present. A 2022 study by ACEP found medical IDs reduce medication errors by 28% in unconscious patients. Real cases show they prevent fatal allergic reactions and dangerous drug interactions.
Can I just write my info on a piece of paper in my wallet?
No. Wallets get lost, ripped open, or left behind during emergencies. First responders don’t search pockets or bags-they check wrists and necks. A bracelet is visible, accessible, and always on you. Paper doesn’t work in a crisis.
Are QR code bracelets safe and private?
Yes. Reputable brands like MedicAlert use encrypted, password-protected profiles. Only emergency responders with a phone and internet access can scan the code. Your data isn’t public. You control who can view it and what’s included.
What if I forget to update my bracelet after changing meds?
Outdated info is dangerous. Set a quarterly reminder. Use a digital profile that syncs with your pharmacy-like MedicAlert’s SmartProfile. It auto-updates when your prescriptions change. That’s the best way to stay safe without remembering every time.
Do insurance companies cover medical alert bracelets?
Most don’t. But some Medicare Advantage plans and HSA/FSA accounts allow you to use pre-tax dollars to buy them. Check with your provider. Even without coverage, the cost is less than one ER visit caused by a preventable error.

Carolyn Benson
December 20, 2025 AT 10:08