Key Takeaways
- Magnesium hydroxide is an antacid and laxative that the kidneys filter and excrete.
- People with reduced kidney function can develop hypermagnesemia if they use magnesium hydroxide incorrectly.
- Monitoring serum magnesium, creatinine, and GFR helps keep use safe.
- Low‑dose, short‑term use is generally safe for healthy adults, but alternatives are better for advanced kidney disease.
- Always discuss dosage with a healthcare professional before starting magnesium hydroxide.
What Is Magnesium Hydroxide?
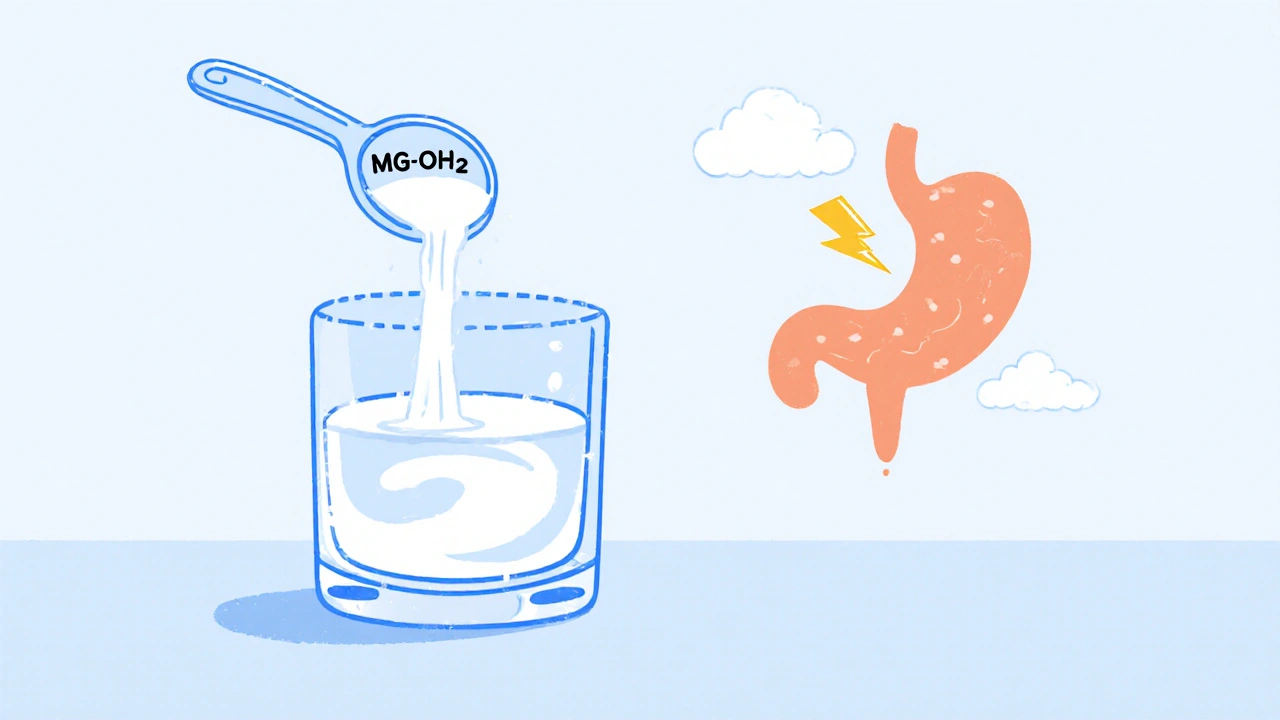
magnesium hydroxide is a white, poorly soluble inorganic compound used as an antacid and laxative. In pharmacies you’ll find it under brand names such as Milk of Magnesia. When mixed with water it forms a milky suspension that neutralizes stomach acid and draws water into the colon, easing constipation.
Because it is not fully absorbed in the gut, most of the dose reaches the bloodstream only in small amounts. Those amounts are then handled by the kidneys, which either re‑absorb or excrete the excess magnesium.
How the Kidneys Handle Magnesium
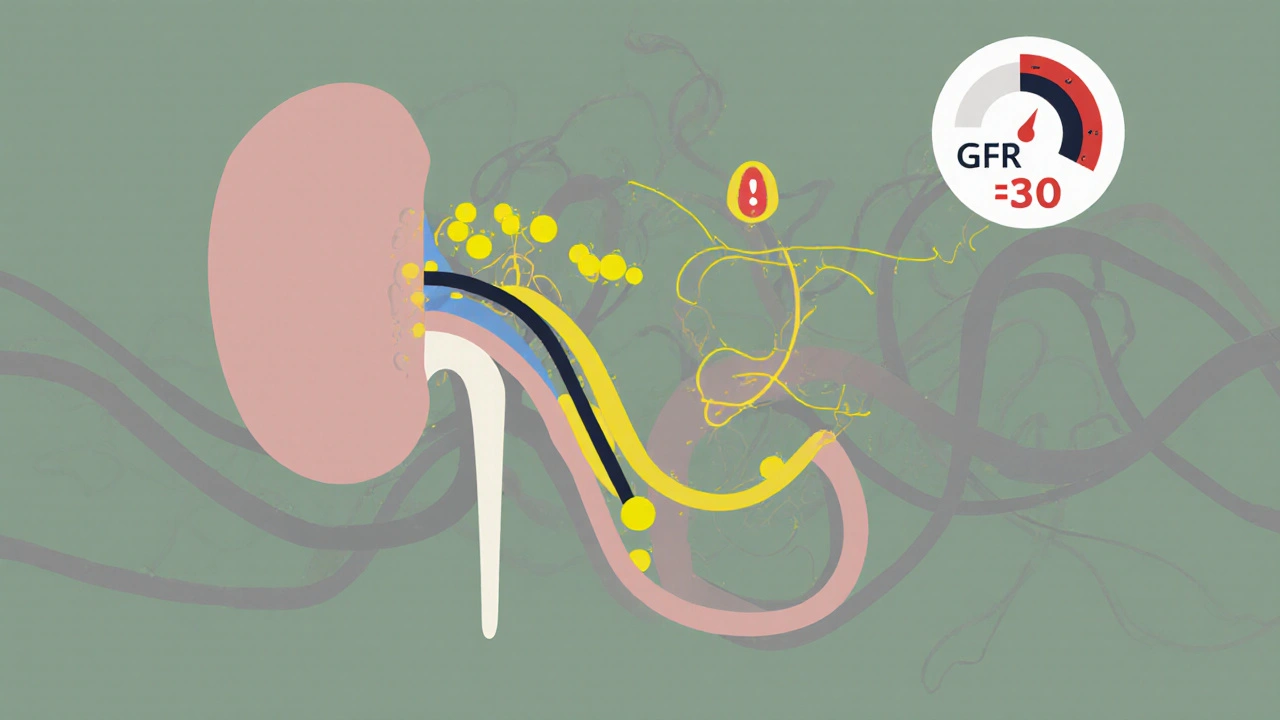
Kidney is a paired organ that filters blood, removes waste, and regulates electrolytes, including magnesium. Each kidney contains about a million nephron is the functional filtration unit of the kidney. Blood enters the glomerulus, a tiny network of capillaries, where waste and excess minerals are sieved out into the tubular system.
Magnesium re‑absorption mainly occurs in the thick ascending limb of the loop of Henle and the distal convoluted tubule. When kidney function drops-measured by the glomerular filtration rate (GFR)-the organ loses its ability to excrete magnesium efficiently, raising the risk of hypermagnesemia.
Why Magnesium Hydroxide Matters for Kidney Health
For most people, occasional use of magnesium hydroxide poses little risk because the kidneys quickly clear the absorbed fraction. However, several scenarios can tip the balance:
- Chronic kidney disease (CKD): As CKD progresses, GFR falls below 30 mL/min, and the kidneys cannot keep up with even modest magnesium loads.
- Concurrent medications: Drugs like calcineurin inhibitors or certain diuretics can impair magnesium excretion.
- High‑dose antacid regimens: Using more than the recommended 2 g daily for several weeks can overwhelm renal clearance.
When excess magnesium accumulates, patients may experience nausea, weakness, low blood pressure, and in severe cases cardiac arrhythmias. Blood tests that show serum magnesium above 2.5 mmol/L combined with rising serum creatinine are red flags.
Assessing the Risk: Key Lab Values
To decide whether magnesium hydroxide is safe, clinicians monitor a few core numbers:
- Serum creatinine is a waste product that reflects kidney filtration efficiency - higher values indicate reduced GFR.
- Glomerular filtration rate (GFR) is the standard measurement of kidney function expressed in mL/min/1.73 m² - a GFR < 30 usually triggers caution.
- Serum magnesium is the concentration of magnesium in the blood, normal range 0.75‑1.0 mmol/L - values > 2.5 mmol/L suggest toxicity.
When any of these markers drift outside safe ranges, doctors often switch patients to non‑magnesium antacids or prescribe stool softeners that do not affect electrolyte balance.
Practical Guidance for Safe Use
If you have normal kidney function (GFR > 60 mL/min), the following plan usually works:
- Start with the lowest effective dose: ½ teaspoon (≈ 1 g) of magnesium hydroxide mixed with water.
- Take it no more than once daily for short‑term relief (≤ 7 days).
- Watch for side effects like loose stools or abdominal cramping; reduce dose if they appear.
For anyone with CKD stage 3‑5 (GFR < 60), consider these alternatives:
- Calcium carbonate - a non‑magnesium antacid that also supplies calcium.
- Aluminum hydroxide - another antacid with minimal systemic absorption.
- Bulk‑forming fiber supplements such as psyllium - they help with constipation without affecting electrolytes.
Always discuss dosage with a healthcare professional before starting any new antacid or laxative regimen.
Comparison Table: Magnesium Hydroxide vs. Common Alternatives
| Attribute | Magnesium Hydroxide | Calcium Carbonate | Aluminum Hydroxide |
|---|---|---|---|
| Primary action | Neutralizes stomach acid; osmotic laxative | Neutralizes stomach acid | Neutralizes stomach acid |
| Systemic absorption | Low, but can raise serum magnesium | Very low; adds calcium | Minimal; aluminium may accumulate in renal failure |
| Best for constipation? | Yes - osmotic effect pulls water into colon | No - may cause constipation | No - neutral effect on bowel movements |
| Kidney safety (CKD stage 3+) | Potential risk of hypermagnesemia | Generally safe; monitor calcium | Risk of aluminium toxicity |
| Typical dose (adult) | 0.5‑2 g per day | 0.5‑1 g per day | 0.5‑1 g per day |
When to Seek Medical Advice
Contact your doctor or a renal specialist if any of the following occur while using magnesium hydroxide:
- Persistent diarrhea lasting more than 48 hours.
- Muscle weakness, tingling, or irregular heartbeat.
- Lab results show serum magnesium > 2.5 mmol/L or creatinine rising > 30 % from baseline.
- You have been on the product for longer than two weeks without improvement.
Early intervention can prevent severe electrolyte disturbances and avoid hospitalization.
Mini‑FAQ
Can magnesium hydroxide improve kidney function?
No. It does not treat kidney disease; it merely supplies magnesium, which the kidneys must clear. In healthy kidneys it’s harmless, but in CKD it can add stress.
Is milk of magnesia safe for dialysis patients?
Dialysis patients often have very low GFR, so most clinicians avoid magnesium hydroxide unless the dose is strictly monitored and serum magnesium is checked after each dose.
How long does it take for the kidneys to clear a dose?
In people with normal renal function, about 50 % of the absorbed magnesium is excreted within 4‑6 hours; complete clearance usually occurs within 24 hours.
What dietary sources add extra magnesium besides supplements?
Leafy greens, nuts, seeds, whole grains, and legumes are rich in magnesium. Eating these foods can often meet daily needs without meds.
Can I take magnesium hydroxide with calcium supplements?
Yes, but the combined calcium and magnesium load can strain the kidneys if you have CKD. Space them out by a few hours and monitor labs.
Bottom Line
For most adults with healthy kidneys, magnesium hydroxide is a handy, low‑cost tool for occasional heartburn or constipation. The key is moderation, short‑term use, and awareness of kidney function. If you already have reduced GFR or are on dialysis, talk to a clinician about safer alternatives and regular blood‑test monitoring.
junior garcia
October 24, 2025 AT 15:20