Opioid Hormone Risk Calculator
How It Works
Based on clinical studies, this calculator estimates your risk of hormonal disruption. Research shows that 63% of men on long-term opioids develop low testosterone. For women, 87% experience menstrual cycle disruption at doses over 60 MME/day.
60-120 MME = Starting point for hormonal effects
Over 120 MME = Higher risk of severe disruption
Your Results
Your estimated risk is N/A
Based on your input
When people start taking opioids for chronic pain, they often focus on one thing: relief. But what they don’t talk about-until it’s too late-is how these drugs quietly shut down their hormones and wreck their sex lives. It’s not a rare side effect. It’s the norm. Studies show that 63% of men on long-term opioid therapy develop low testosterone. For women, menstrual cycles often vanish. Libido drops. Erectile dysfunction becomes routine. And most doctors never mention it until the patient brings it up.
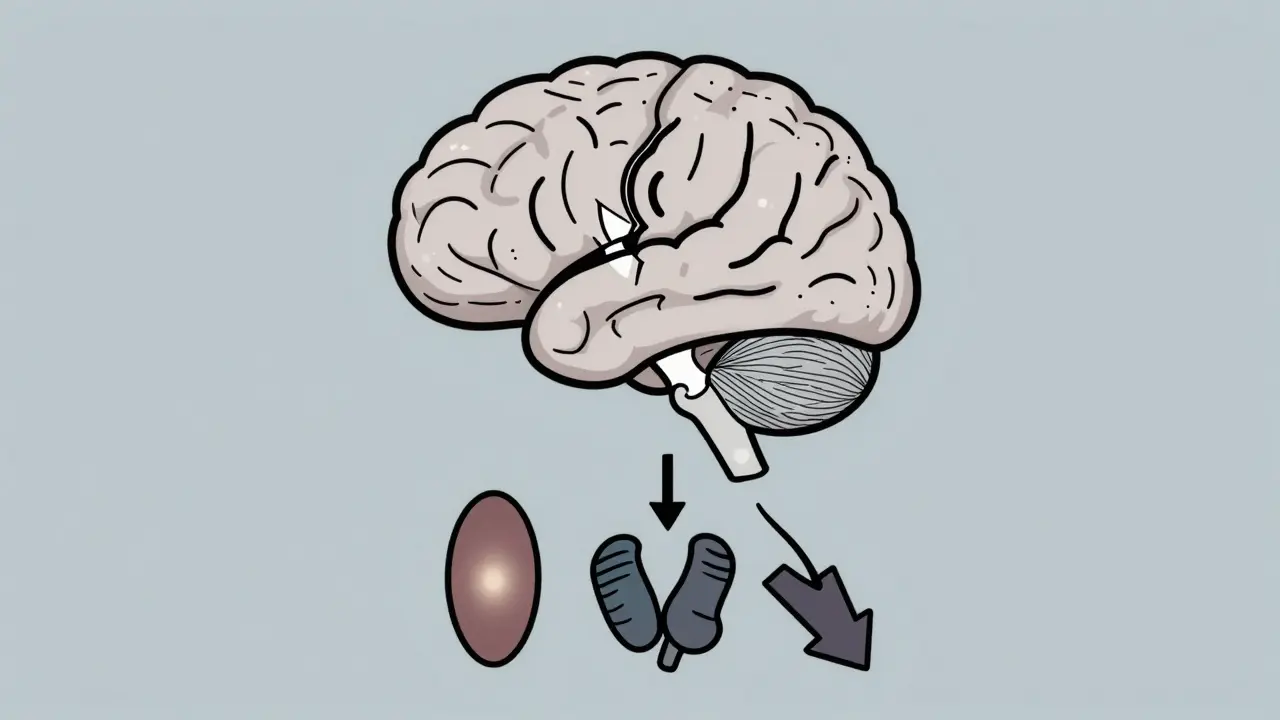
How Opioids Break Your Hormones
Opioids don’t just block pain signals. They also block your brain’s ability to tell your body how to make sex hormones. The system that controls this is called the hypothalamic-pituitary-gonadal (HPG) axis. It’s like a factory: the hypothalamus sends a signal, the pituitary gland responds, and the testes or ovaries make testosterone or estrogen. Opioids jam the signal at the very start. No signal means no hormone production.It happens fast. Within 30 days of starting daily opioids, testosterone levels in men can drop by 30% to 50%. By six months, two out of three men are clinically hypogonadal-meaning their testosterone falls below 300 ng/dL. That’s not just low. That’s the level you’d expect in a 70-year-old man, not a 40-year-old.
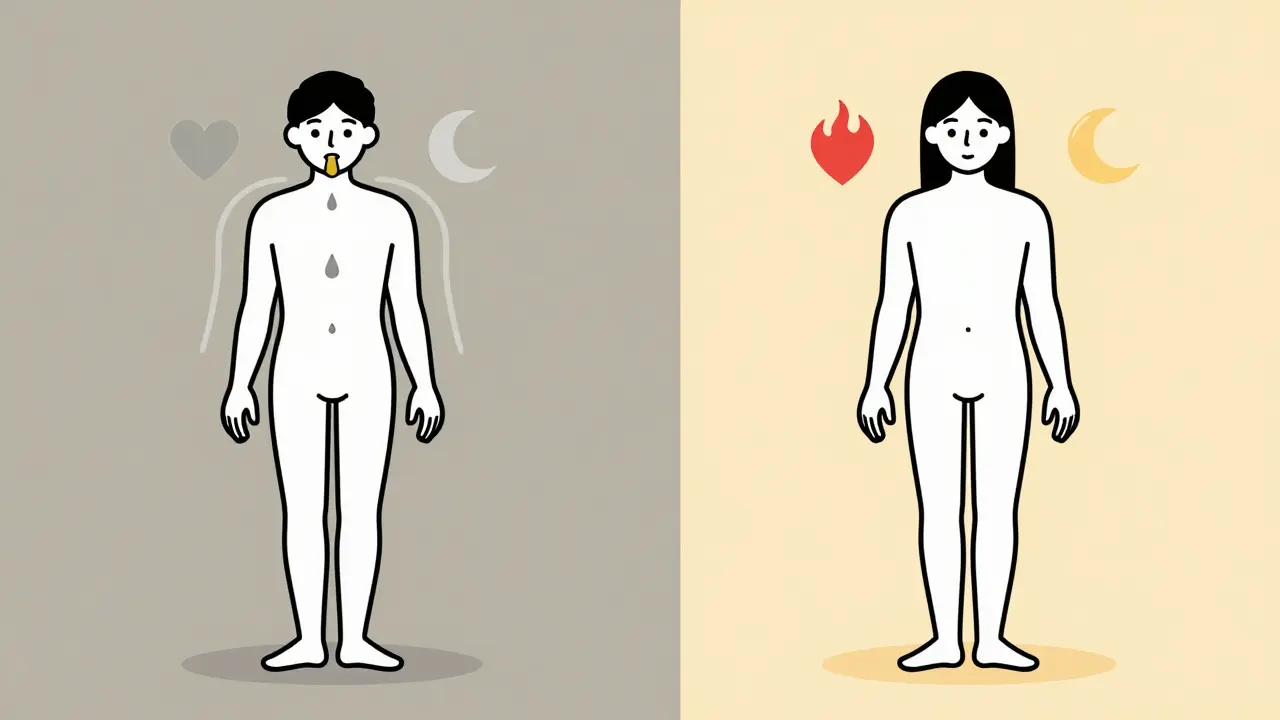
For women, the story is different but just as serious. Estradiol (the main female hormone) often stays normal, but free testosterone-the kind that drives libido-plummets. One study found that 87% of premenopausal women on long-term opioids had messed-up periods. Nearly one in five stopped menstruating entirely. Another third had unpredictable cycles. These aren’t random changes. They’re direct results of opioid interference.
What Dose Does the Damage?
You don’t need to be on high doses to feel this. The damage starts at 60-120 morphine milligram equivalents (MME) per day. That’s roughly:- Two 30 mg oxycodone pills daily
- One 10 mg hydrocodone tablet three times a day
- One 25 mcg/hour fentanyl patch
At doses above 120 MME, nearly every patient shows signs of hormonal disruption. But even people on lower doses aren’t safe. A 2020 meta-analysis found that 21% to 86% of all chronic opioid users-men and women-had measurable hormone imbalances. That’s not a small group. That’s most people on long-term therapy.
Sexual Function Takes a Hit
Low testosterone doesn’t just mean less muscle or energy. It means less desire, less performance, and less pleasure.In men, the most common complaints are:
- Loss of libido (reported by 89% of Reddit users on chronic opioids)
- Erectile dysfunction (up to 75% of cases)
- Reduced sperm count and fertility
- Depression and fatigue that feel worse than the original pain
One user on a chronic pain forum wrote: “I was on oxycodone for two years. My doctor never tested my testosterone. I didn’t know why I felt so drained until I found out it was 180 ng/dL. Took six months to get treatment.”
For women, the impact is just as real but less talked about:
- 78% reported decreased sex drive
- 63% had irregular or absent periods
- 41% said their depression got worse
Many women were told their symptoms were just “part of chronic pain” or “normal aging.” But the data doesn’t lie. This is opioid-induced endocrinopathy. It’s a medical condition, not a side effect you have to live with.
How Other Painkillers Compare
Not all pain meds do this. Opioids are the worst offenders.Compare this:
| Treatment | Testosterone Drop in Men | Menstrual Issues in Women | Sexual Dysfunction Rate |
|---|---|---|---|
| Opioids (chronic use) | 63% | 87% | 21-86% |
| Gabapentinoids (e.g., pregabalin) | 12% | Not studied | 5-10% |
| NSAIDs (e.g., ibuprofen) | Minimal | Minimal | 5-15% |
| Cognitive Behavioral Therapy | None | None | None |
Non-opioid options like physical therapy, CBT, or even certain antidepressants (like duloxetine) don’t touch your hormones. They might take longer to work, but they don’t break your body the way opioids do. The American Pain Society and CDC both warn against using opioids as first-line treatment for chronic non-cancer pain-precisely because of these hidden harms.
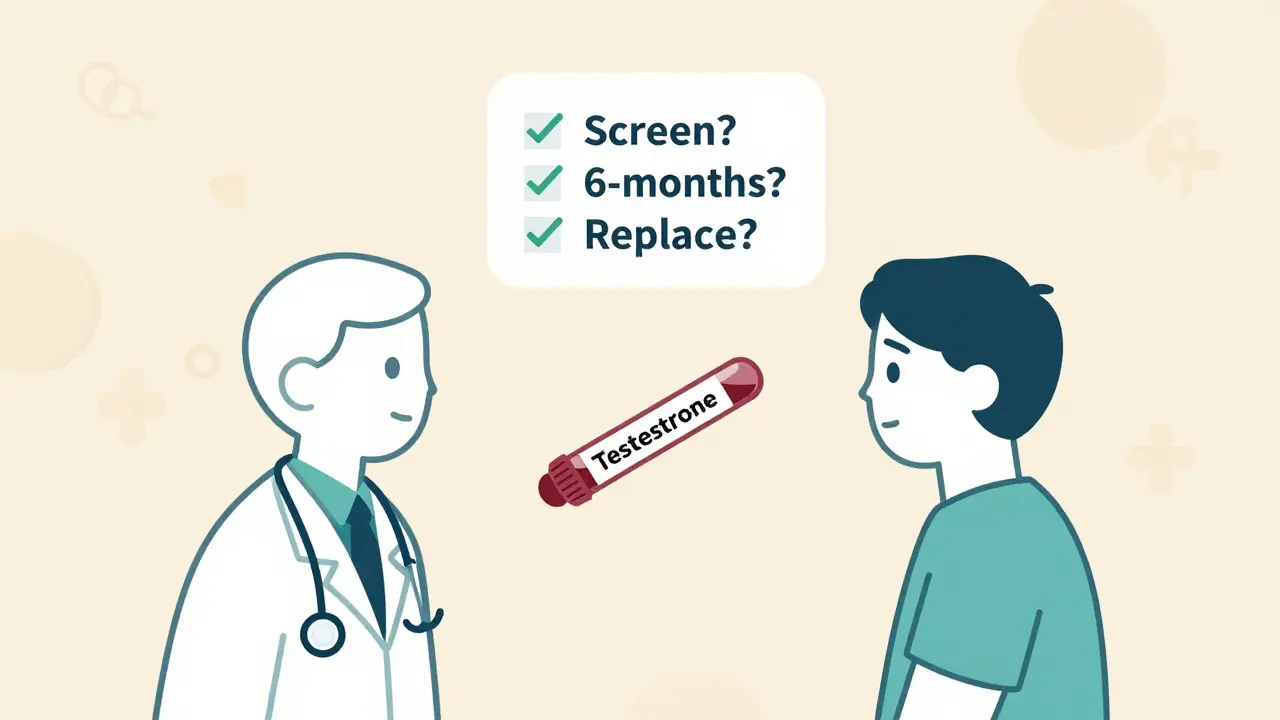
What Doctors Should Do (But Often Don’t)
The Endocrine Society’s 2019 guidelines say this plainly: “Testosterone screening should be routine for all men on chronic opioid therapy.” And yet, a 2023 study found only 38% of primary care doctors do it. That’s not just negligence. It’s substandard care.Here’s what should happen:
- Before starting opioids, test baseline testosterone in men and menstrual history in women.
- Repeat testing every 6 months.
- If testosterone is low (<300 ng/dL), consider replacement therapy.
- For women with amenorrhea or low libido, explore off-label testosterone patches (1-2 mg daily).
- Never assume symptoms are just “depression” or “aging.”
And here’s the kicker: testosterone replacement therapy works. When levels are restored, 70-85% of men see improvement in libido, energy, and erectile function. It’s not a magic fix, but it’s the only fix that addresses the root cause.
What About Women? Why Is There So Little Research?
Here’s the ugly truth: most opioid studies were done on men. Female patients were rarely included. A 2023 review in the Journal of Women’s Health found that only 2% of opioid trials looked at female sexual function.That means we’re flying blind. We know low testosterone affects women’s libido. We know estrogen stays stable. But we don’t have clear guidelines for treatment. Some doctors use testosterone patches. Others try SSRIs or counseling. But there’s no standard. And that’s dangerous.
Women need to ask for testing. They need to demand answers. If your period stops or your sex drive vanishes while on opioids, it’s not normal. It’s a red flag.
The New Hope: Safer Alternatives
There’s progress. In 2023, the FDA approved Belbuca (buprenorphine buccal film), which causes 40% less hormone disruption than traditional opioids. Cleveland Clinic’s 2024 study showed that combining low-dose naltrexone with reduced opioid dosing improved testosterone levels by 25-35% in 68% of patients-without losing pain control.And the market is shifting. The non-opioid pain management industry is growing at nearly 9% per year. Testosterone replacement therapy is booming too, partly because of opioid-induced hypogonadism. But the real win? When doctors treat the whole person-not just the pain.
One patient told me: “My pain specialist didn’t care about my sex life. My endocrinologist did. Once I got my testosterone up, I felt like myself again. Not just numb. Not just in pain. Me.”
What You Can Do
If you’re on long-term opioids:- Ask for a testosterone blood test-even if you feel fine.
- Track your libido, erections, or menstrual cycles. Write it down.
- Don’t accept “it’s just depression” as an answer.
- Ask about non-opioid alternatives: physical therapy, nerve blocks, CBT, or acupuncture.
- If you’re considering tapering off opioids, don’t do it alone. Withdrawal can be brutal. 73% of people who try without help go back to their old dose within 90 days.
The goal isn’t to scare you. It’s to empower you. You deserve pain relief without losing your body, your energy, or your intimacy. Opioids aren’t evil. But they’re not the answer for most long-term pain. And you have the right to know the full cost.
Do all opioids affect hormones the same way?
No. While all opioids suppress the HPG axis, some have stronger effects. Morphine, oxycodone, and fentanyl are the worst offenders. Buprenorphine (especially in buccal film form) shows significantly lower disruption-about 40% less than traditional opioids. Short-acting opioids may be slightly less damaging than long-acting ones, but the difference isn’t enough to make them safe for long-term use.
Can I just take testosterone supplements without stopping opioids?
Yes, but it’s not a full solution. Testosterone replacement therapy (TRT) can restore libido, energy, and mood in men with low levels. But it doesn’t fix the root problem: opioids are still shutting down your natural hormone production. TRT also carries risks like polycythemia (thick blood), sleep apnea, and prostate issues. It’s a band-aid. The better path is reducing opioid dose while using TRT as a bridge-under medical supervision.
Why don’t doctors talk about this?
Many don’t know. Others avoid it because they think it’s too uncomfortable or irrelevant. A 2023 JAMA Internal Medicine study found only 38% of primary care doctors routinely screen for opioid-induced hormone problems. There’s also stigma-patients don’t bring it up, so doctors don’t ask. But experts like Dr. Bolash from Cleveland Clinic say: “If you don’t ask, you’re missing half the patient’s experience.”
Is hormone damage permanent?
Usually not. Once opioids are reduced or stopped, hormone levels often bounce back within 3-6 months. But if opioids are used for years without intervention, some damage may linger. Early detection and treatment are key. Men who start TRT early and taper opioids safely have the best recovery rates. Women who get help for menstrual disruption often resume normal cycles after reducing opioid use.
What are the best alternatives to opioids for chronic pain?
For most people, the best options are non-drug therapies: physical therapy, cognitive behavioral therapy (CBT), acupuncture, and mindfulness-based stress reduction. Medications like gabapentin, pregabalin, or certain antidepressants (duloxetine, amitriptyline) can help nerve pain. NSAIDs work well for inflammatory pain. Injections (nerve blocks, epidurals) and spinal cord stimulators are also effective for specific conditions. None of these cause hormone disruption.