When a vertebra in your spine cracks under pressure - often from osteoporosis, a fall, or cancer - the pain can be unbearable. Standing, sitting, even breathing becomes hard. For many older adults, this isn’t just a minor injury. It’s life-changing. That’s where kyphoplasty and vertebroplasty come in. These aren’t big, open surgeries. They’re quick, minimally invasive procedures that can turn your pain from an 8 out of 10 down to a 2 in just hours. But which one is right for you? And does the extra cost of kyphoplasty actually make a difference?
What Exactly Happens in These Procedures?
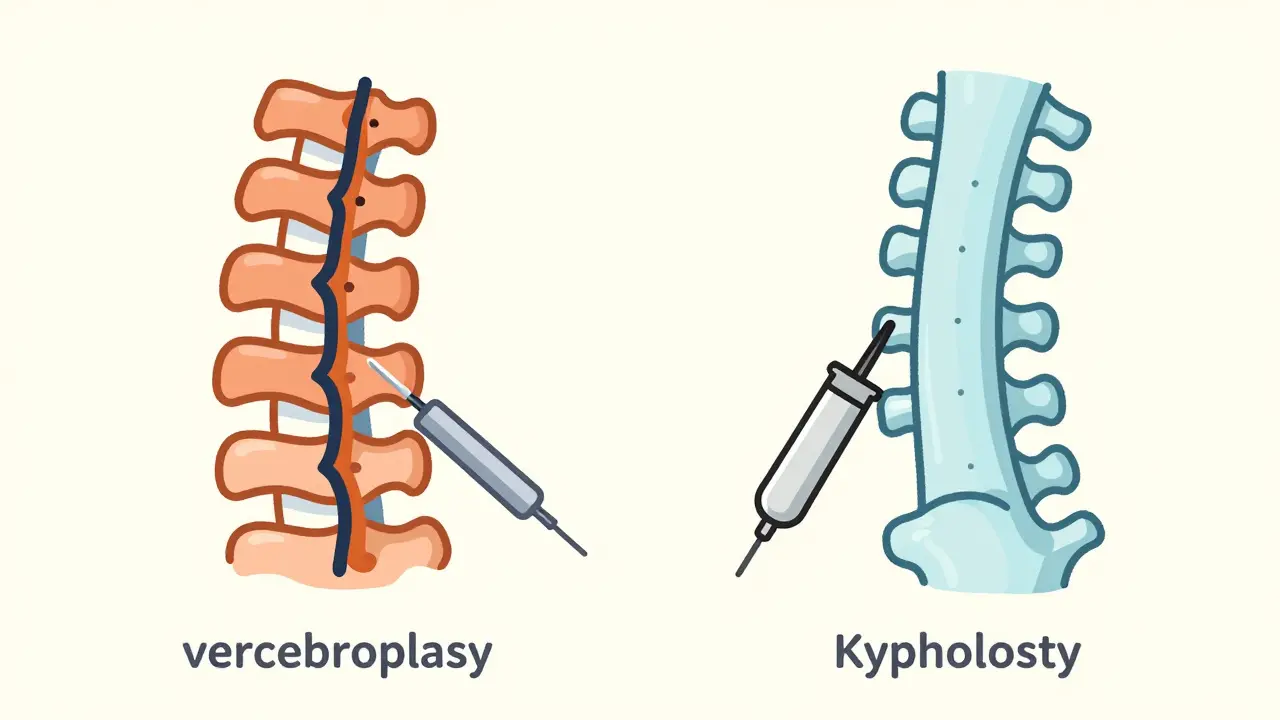
Both kyphoplasty and vertebroplasty fix broken spinal bones using a special bone cement called polymethylmethacrylate (PMMA). The goal? To stabilize the fracture, stop the pain, and help you move again. You lie face down, get local anesthesia and light sedation, and a thin needle is guided into the fractured vertebra using real-time X-ray imaging. The cement is injected, hardens in 10 to 20 minutes, and acts like an internal cast.The big difference? Kyphoplasty adds a balloon step. Before the cement goes in, a small balloon is inserted into the broken bone and gently inflated. This lifts the collapsed vertebra back toward its original shape, creating a cavity. Then the balloon is popped out, and the cement is pumped in. Vertebroplasty skips the balloon. The cement is injected directly into the fracture under higher pressure, filling cracks and gaps in the bone.
That balloon step isn’t just for show. It’s why kyphoplasty can restore lost height in the spine - something vertebroplasty rarely does. In studies, kyphoplasty can bring back 40 to 60% of the height lost from the fracture. Vertebroplasty? It mostly just fills the gap. No real lift.
Which One Gives Better Pain Relief?
Here’s the surprising part: both work almost equally well for pain.Studies show 85 to 90% of patients report major pain reduction within 24 hours after either procedure. Pre-procedure pain scores average 8.2 on a 10-point scale. After? Down to 1.5. That’s not a small change. That’s life-changing. Whether you get the balloon or not, most people stop needing strong painkillers within a week. One patient on Reddit said it felt like flipping a switch - pain gone, just like that.
So if pain relief is your main goal, both procedures deliver. But if you’re worried about your posture - if you’ve developed a hunched back from multiple fractures - kyphoplasty has an edge. It can straighten things out a bit. Vertebroplasty won’t fix that.
What About Risks and Complications?
No procedure is risk-free. The biggest concern with both is cement leaking out of the bone. This can happen into nearby tissues, nerves, or even blood vessels.Vertebroplasty has a higher leak rate - anywhere from 27% to 68% of cases. But most of these leaks don’t cause symptoms. Only about 1.1% lead to serious problems like nerve damage or a pulmonary embolism.
Kyphoplasty cuts that risk in half. With the balloon creating a controlled space, cement leakage drops to 9% to 33%. That’s a big deal for older patients with fragile bones. The balloon gives the surgeon more control. Less pressure means less chance of cement sneaking where it shouldn’t.
Another risk? New fractures nearby. About 5 to 10% of patients develop a fracture in a neighboring vertebra within a year. That’s not because the procedure caused it - it’s because the rest of the spine is still weak from osteoporosis. That’s why treating the root cause - bone density - is just as important as fixing the broken bone.
Cost and Insurance: Is Kyphoplasty Worth the Extra Money?
Kyphoplasty costs about 20 to 30% more than vertebroplasty. In the U.S., Medicare pays around $3,850 for kyphoplasty versus $2,950 for vertebroplasty. That’s a $900 difference per procedure.Does that extra cost buy you better results? For pain relief? No. For restoring height? Yes. But here’s the catch: research shows that height restoration doesn’t always mean better long-term function. A 2007 study found that the height gained during kyphoplasty dropped by 30% after just 500 body movements - basically, the spine settles back down.
Some doctors argue vertebroplasty is the smarter choice for simple fractures without major deformity. It’s cheaper, just as effective for pain, and has a shorter learning curve for surgeons. Others say kyphoplasty’s lower leak rate and potential for posture correction make it worth the price - especially for younger, more active patients or those with multiple fractures.
Medicare covers both procedures if you’ve tried at least 4 to 6 weeks of rest, pain meds, and physical therapy without improvement. Approval rates are above 95% when paperwork is in order.
Who Gets These Procedures?
Most patients are over 65. Women make up 70 to 75% of cases because osteoporosis hits them harder after menopause. About 25% of women over 50 and 40% over 80 will have at least one osteoporotic spinal fracture in their lifetime. That’s over 700,000 fractures a year in the U.S. alone.Kyphoplasty is now the most common choice - about 65% of all vertebral augmentations. That’s because of its safety profile and the fact that many hospitals have standardized on it. But vertebroplasty is still widely used, especially in smaller centers or for patients who can’t afford the higher cost.
Not everyone qualifies. If your fracture is old - more than 6 to 8 weeks - and there’s no swelling or fluid in the bone (seen on MRI), neither procedure will help. The cement needs active inflammation to stick properly. Chronic fractures? They need other treatments.
What’s New in 2026?
The field is evolving. New cement types - like calcium phosphate - are being used because they mimic natural bone better and generate less heat during hardening. That reduces the risk of burning nearby nerves.A major 2023 study in The Lancet found that getting treated within two weeks of a fracture cut 12-month death risk by 28%. That’s huge. It suggests these aren’t just pain fixes - they’re life-saving. Early intervention matters.
Right now, a large trial called COAST is tracking patients for two years to see if kyphoplasty’s height restoration leads to real improvements in walking, standing, or daily function. So far, the data doesn’t show a clear advantage. But the hope is that for some patients - especially those with severe deformity - it might.
Industry analysts predict kyphoplasty will make up 75% of all vertebral procedures by 2028. Why? Not just because it’s better - but because it’s seen as safer. And in aging populations, safety matters.
What to Expect After the Procedure
You’ll be monitored for 4 to 6 hours after the procedure. Most people go home the same day. You’ll need to avoid heavy lifting for a week. Walking is encouraged - it helps circulation and prevents blood clots.Many patients report feeling better within hours. Some say they could finally sleep through the night. Others say they could bend over to tie their shoes again. That’s the real win.
But here’s the catch: the procedure fixes the broken bone. It doesn’t fix osteoporosis. If you don’t start taking calcium, vitamin D, and bone-strengthening meds like bisphosphonates, you’re at high risk for another fracture. That’s why follow-up with your doctor or an osteoporosis specialist is non-negotiable.
Real Patient Stories
One woman in her 78s, who had three spinal fractures over two years, had vertebroplasty on her first fracture. She said the pain dropped from a constant 7 to a mild 3. But her posture didn’t improve. She still hunched over.When she had kyphoplasty on her next fracture, she noticed the difference. “I stood up straighter,” she told her doctor. “Not perfect, but better. And I didn’t feel like I was falling forward anymore.”
Another man, 72, had kyphoplasty after a fall. He went from needing a walker to walking without aids in under a week. “I didn’t think I’d ever get back to gardening,” he said. “Now I’m planting tomatoes again.”
But not everyone has a smooth ride. About 10 to 15% of patients say their pain didn’t fully go away. Some develop new fractures nearby. A few report numbness or tingling - usually temporary, but sometimes lasting.
What’s clear? These procedures aren’t magic. But for the right person, at the right time, they’re one of the most effective tools we have to get people back on their feet.
Is kyphoplasty better than vertebroplasty?
It depends on your situation. Kyphoplasty is better if you have significant spinal deformity or height loss because it can restore some of that height and has a lower risk of cement leakage. But for simple fractures without deformity, vertebroplasty works just as well for pain relief and costs less. Both are effective - the choice often comes down to fracture type, patient age, and cost considerations.
How long does it take to recover from kyphoplasty or vertebroplasty?
Most patients go home the same day. You’ll feel better within hours, but full recovery takes 1 to 2 weeks. You should avoid heavy lifting and twisting for at least 6 weeks. Walking is encouraged right away. Many people return to normal daily activities within 72 hours.
Do these procedures cure osteoporosis?
No. These procedures fix the broken bone, but they don’t treat the underlying bone weakness. If you don’t start taking calcium, vitamin D, and osteoporosis medications like bisphosphonates or denosumab, you’re at high risk for another fracture. Managing osteoporosis is just as important as the procedure itself.
Are these procedures covered by insurance?
Yes. Medicare and most private insurers cover both kyphoplasty and vertebroplasty if you’ve tried at least 4 to 6 weeks of conservative treatment - like rest, pain meds, and physical therapy - without improvement. Approval rates are over 95% when documentation is complete.
Can I have this procedure if I’m over 80?
Absolutely. In fact, most patients are over 65, and about 40% of women over 80 have had at least one spinal fracture. Age alone isn’t a barrier. What matters more is your overall health, bone quality, and whether the fracture is recent (less than 6 to 8 weeks old). Many older adults regain mobility and independence after the procedure.
What happens if the cement leaks?
Cement leakage is common - especially with vertebroplasty - but most leaks cause no symptoms. If cement leaks into a nerve space or blood vessel, it can cause pain, numbness, or even a pulmonary embolism. This is rare (under 1.5% of cases) and more likely with vertebroplasty. Kyphoplasty reduces this risk because the balloon creates a controlled space for the cement. Surgeons monitor for leaks in real time during the procedure.
How long does the cement last?
The cement is permanent. Once it hardens, it stays in place for life. But the surrounding bone may continue to weaken from osteoporosis. That’s why ongoing treatment for bone health is critical. The cement doesn’t prevent future fractures - it only stabilizes the one that’s already broken.
