If you're taking medication for anxiety, sleep, or pain - and you're also using kava - you could be putting your liver at risk. It's not just a theoretical concern. Real people have ended up in the hospital, some needing liver transplants, after mixing kava with their prescription sedatives. The FDA has warned about this since 2002. Yet, kava is still sold freely in the U.S. as a dietary supplement, often without any clear warning labels. Many users assume it's safe because it's "natural." That’s a dangerous myth.
What Exactly Is Kava?
Kava, also called kava kava, comes from the roots of the Piper methysticum plant, traditionally used in Pacific Island ceremonies for its calming effects. Today, it’s sold as capsules, powders, teas, and liquid extracts, mostly marketed for anxiety relief. Its active ingredients, called kavalactones, interact with brain receptors to reduce stress and muscle tension. A typical dose ranges from 70 to 250 mg of kavalactones per day. Traditional Pacific preparations use water to extract these compounds, resulting in a mild, earthy drink. But most commercial products - especially those sold online - use alcohol or acetone to pull out more kavalactones, creating a much stronger, more concentrated product. That’s where things get risky.
Why Kava Can Hurt Your Liver
Over 25 international cases of severe liver injury linked to kava have been documented. Some led to liver failure and transplant. The exact mechanism isn’t fully understood, but researchers believe kavalactones interfere with liver enzymes - specifically CYP2D6, CYP2C9, and CYP3A4 - that your body uses to break down toxins and medications. When these enzymes are blocked, harmful substances build up in the liver. This isn’t just a guess. The California Department of Public Health confirmed this interaction in 2024. Even more troubling: kava doesn’t always cause problems right away. Symptoms like fatigue, nausea, dark urine, or yellowing skin can take weeks or months to appear. By then, damage may already be advanced.
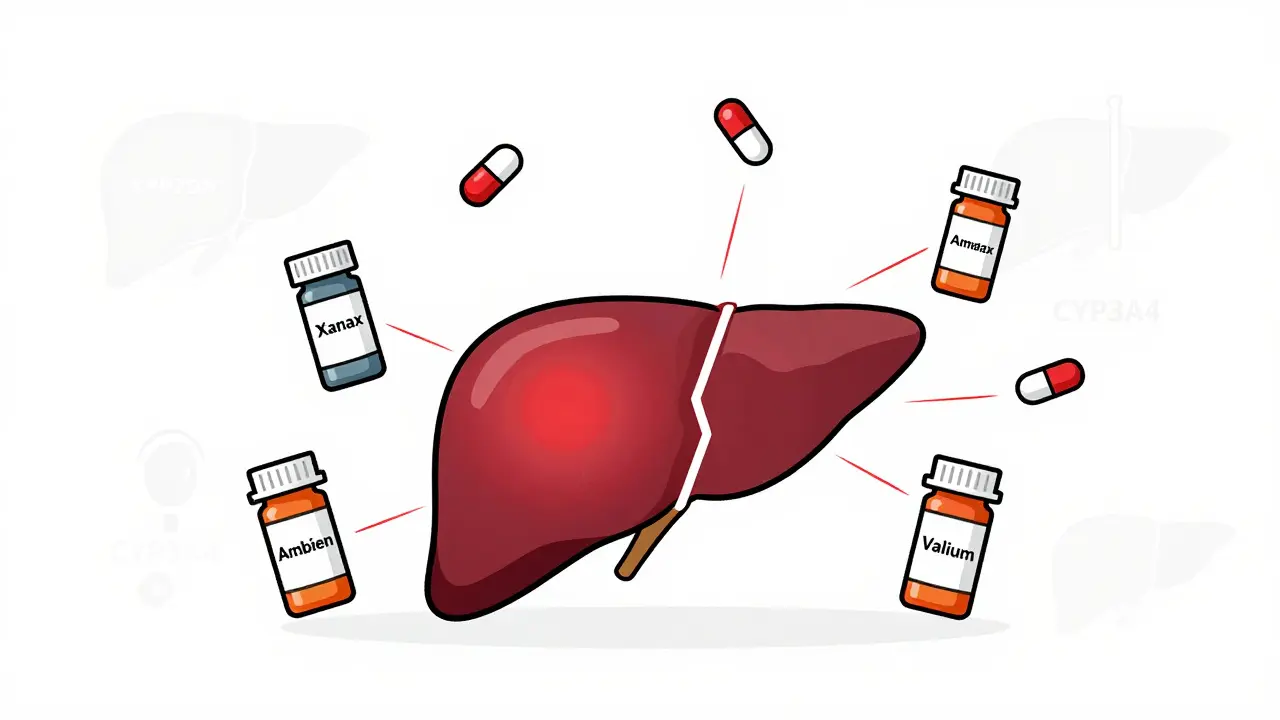
The Bigger Danger: Mixing Kava With Sedatives
Kava doesn’t just stress your liver - it also makes sedative medications stronger. If you’re taking benzodiazepines like alprazolam (Xanax), diazepam (Valium), or lorazepam (Ativan), or sleep aids like zolpidem (Ambien), combining them with kava can turn a normal dose into an overdose. One Sacramento County case study in 2023 showed a 42-year-old woman taking 300 mg of kava daily with 2 mg of alprazolam developed jaundice and liver enzymes over 2,800 U/L - more than 10 times the normal level. Another patient, on diazepam and kava, had a blood clotting factor (INR) of 4.2, putting him at high risk of internal bleeding.
WebMD rates kava’s interaction with benzodiazepines as "Major." Studies show kava can increase midazolam levels in the blood by 27%. That’s not a small bump - it’s enough to cause extreme drowsiness, confusion, slowed breathing, or even unconsciousness. Reddit users have shared stories of being unable to stand for hours after combining kava with lorazepam. One wrote: "I couldn’t speak clearly. I thought I was having a stroke." These aren’t rare outliers. The FDA’s adverse event database recorded 37 sedation-related incidents involving kava between 2019 and 2023 - 12 of them required emergency care.
How Kava Compares to Other Herbal Supplements
Not all herbal remedies are the same. Valerian root, often used for sleep, has almost no documented drug interactions. Ashwagandha might affect thyroid or blood pressure meds, but it doesn’t reliably inhibit liver enzymes like kava does. Kava stands out because of its dual threat: liver toxicity and CNS depression. Even compared to prescription anxiety drugs, kava is unpredictable. Alprazolam has a severe liver injury rate of about 1 in 100,000 prescriptions. Kava’s estimated rate is lower - around 1 in 1,000,000 daily doses - but that number is likely underreported. Unlike prescription drugs, kava supplements aren’t tested for consistency. One bottle might have 100 mg of kavalactones; the next might have 300 mg. No standardization. No quality control.

Who Should Avoid Kava Completely?
There are clear red flags. If you have any history of liver disease - hepatitis, fatty liver, elevated liver enzymes - don’t touch kava. The CDC says it’s not worth the risk. If you’re on any medication metabolized by the liver - especially sedatives, antidepressants, antifungals, or statins - you should avoid it. Even if you’re healthy, if you drink alcohol regularly, combining it with kava multiplies the risk of liver damage. Australia’s Therapeutic Goods Administration warns that long-term use of doses over 250 mg daily increases risk. And if you’re over 60, your liver processes toxins slower, making you more vulnerable.
What If You’ve Already Been Taking Kava?
Don’t panic, but don’t ignore it either. Stop taking kava immediately if you notice any of these symptoms: unusual tiredness, loss of appetite, nausea, dark urine, or yellow eyes or skin. Get a liver function test. The American Association for the Study of Liver Diseases says if your ALT levels rise above three times the normal upper limit, you must stop kava. In 92% of mild cases, liver enzymes return to normal within two months after quitting. But if you keep going, you could be risking irreversible damage.
What Healthcare Providers Need to Know
Most patients won’t mention kava unless directly asked. Sacramento County researchers found only 22% of people with liver problems volunteered that they were using it. Doctors and pharmacists need to make kava a standard part of medication reviews. Ask: "Are you taking any herbal supplements or natural remedies?" Don’t assume it’s harmless. Pharmacists should screen for 14 major interactions - especially with haloperidol (risk of heart rhythm problems), ropinirole (risk of low blood pressure), and alcohol. If a patient is on sedatives and using kava, recommend stopping the supplement. If they insist on continuing, insist on biweekly liver tests and cap intake at 70 mg daily.
The Regulatory Mess
Kava is banned as a medicine in the EU, Canada, the UK, and Switzerland. In the U.S., it’s sold as a supplement under the 1994 Dietary Supplement Health and Education Act, which means the FDA can’t require proof of safety before it hits shelves. The FDA issued a warning in 2002 - and still hasn’t taken action to restrict sales. In 2024, California issued formal warnings about kava’s liver risks. New York is considering a bill that would require warning labels. Meanwhile, the global kava market hit $117 million in 2022, with 68% of U.S. sales happening online - where no one checks your meds or asks about your liver. Naturopathic doctors still recommend kava to 41% of their patients, while only 3% of board-certified psychiatrists do.
Is There a Safer Way?
Emerging research suggests traditional water-based kava, like what’s prepared in the Pacific Islands, may be safer than alcohol-extracted supplements. The World Health Organization’s 2023 report found that water-prepared kava had 9 times fewer adverse events than commercial extracts. Some researchers believe noble kava varieties - traditionally used in ceremonies - contain fewer toxic compounds than "two-day" varieties bred for higher potency. But until we have standardized, regulated products, it’s impossible to know what’s in your bottle. If you want to use kava for anxiety, consider talking to a mental health professional. There are proven, safe alternatives: therapy, SSRIs, mindfulness, and exercise all have strong evidence behind them.
Bottom Line
Kava isn’t a harmless herbal tea. It’s a potent substance that can damage your liver and dangerously amplify the effects of sedatives. The risks aren’t theoretical - they’re documented in hospitals and medical journals. If you’re taking any medication that makes you drowsy, avoid kava. If you’ve been using it and feel off, get your liver checked. And if you’re a healthcare provider, ask about it. No one should be surprised by liver failure because no one asked the right question.
Brandon Boyd
December 31, 2025 AT 03:32