When a child can’t swallow a pill, or an adult is allergic to a dye in a standard medication, compounding saves lives. But when it goes wrong, it can kill. In 2022, the FDA reported 27 cases of fentanyl overdose tied to mislabeled compounded pain creams - all preventable. These aren’t rare mistakes. Studies show 3% to 15% of compounded medications have strength errors. That’s not a glitch. That’s a system failure. And it’s happening because too many pharmacies skip the basics.
Know the Rules - USP <795>, <797>, and <800> Aren’t Suggestions
There’s no room for guesswork in compounding. The USP <795> is the baseline for non-sterile preparations - things like topical creams, oral liquids, or capsules. If you’re mixing a gluten-free levothyroxine suspension for a toddler, you need a clean room with ISO Class 8 air quality. No exceptions. The USP <795> standard requires dedicated areas, proper ventilation, and documented cleaning procedures. Skip this, and you’re inviting mold, bacteria, or cross-contamination.
For sterile products - injections, IV bags, eye drops - USP <797> is non-negotiable. This means ISO Class 5 cleanrooms, laminar airflow hoods, and staff wearing full sterile garb. A single airborne particle can cause sepsis. The 2012 NECC outbreak, which killed 64 people, happened because they skipped sterile technique. That’s not history. It’s a warning.
And if you’re handling chemo drugs, hormones, or other hazardous substances, USP <800> applies. You need ventilated cabinets, spill kits, and staff trained in PPE use. Ignoring <800> doesn’t just risk patient safety - it risks your license.
Dual-Check Everything - No Exceptions
One pharmacist calculates a dose. Another verifies it. That’s the rule. Not a suggestion. Not when it’s busy. Not when you’re tired. The American Society of Health-System Pharmacists (ASHP) says dual verification cuts errors by over 50%. In one 2021 study, 78% of compounded medication errors happened because only one person checked the math.
It’s not just calculations. Every ingredient needs two checks. The vial says ‘lidocaine 10%’. Is it lidocaine? Is it 10%? Is it the right lot? Use FTIR or HPLC for confirmation if you can. If you can’t, use a second pharmacist to visually verify the label, container, and powder against the prescription. Document both signatures. No shortcuts.
Even the most experienced pharmacists make mistakes. A 2023 survey found that 31% of errors occurred in pharmacists with over 15 years of experience. Fatigue, distraction, and overconfidence are the real enemies - not lack of skill.
Labeling Isn’t Just a Formality - It’s a Lifeline
One wrong decimal point. One misread ‘mg/mL’ as ‘mg/container’. That’s what happened to a 78-year-old woman in Ohio in 2021. She got a compounded tramadol solution labeled ‘50 mg per container’ - but the container held 100 mL. She took 50 mg thinking it was a single dose. It was 5,000 mg. She ended up in ICU.
The FDA’s 2023 draft guidance now requires all compounded labels to use concentration units only: ‘mg/mL’, not ‘per dose’, ‘per vial’, or ‘per bottle’. This isn’t bureaucracy. It’s survival. Labels must include:
- Active ingredient(s) and strength (mg/mL)
- Beyond-use date (BUD)
- Storage instructions
- Pharmacy name and phone number
- Lot number and batch record ID
And don’t rely on handwriting. Print labels. Use barcodes. Scan them during verification. A 2021 study at the University of Tennessee showed barcode scanning reduced ingredient misidentification by 92%.

Track Your Beyond-Use Dates - Or Risk Patient Harm
Compounded meds don’t come with expiration dates like factory-made drugs. You set the beyond-use date (BUD). And you’re responsible for getting it right.
For non-sterile preparations like oral suspensions, BUDs range from 30 to 180 days, depending on the base, preservatives, and storage. A sugar-based suspension might last 30 days at room temperature. A glycerin-based one? Up to 180. But if you don’t test it, you’re guessing.
Sterile products are even tighter. An IV bag made in a cleanroom might be good for 45 days if refrigerated. If it’s left out? 24 hours. The Joint Commission found that 23% of compounding errors involved expired or improperly stored products.
Keep a log. Test stability. Document everything. Don’t assume. Don’t copy someone else’s BUD. Every formula is different.
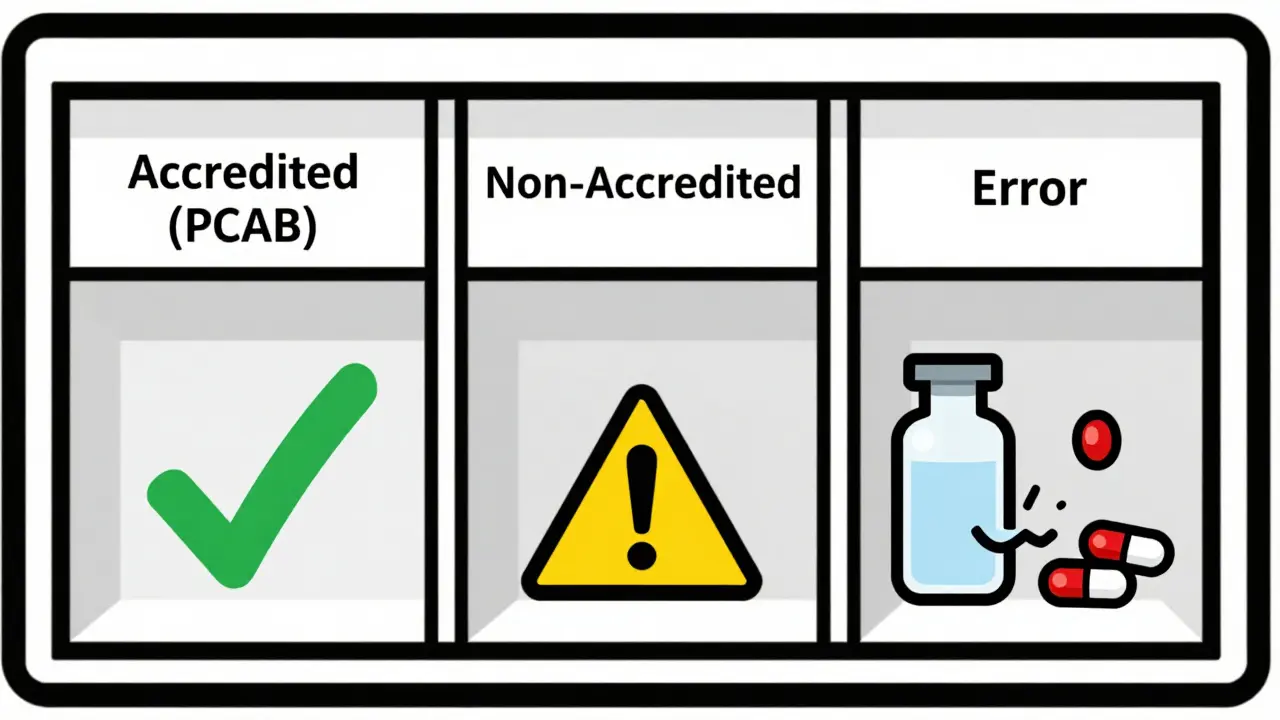
Accreditation Isn’t Optional - It’s Your Shield
Only 18% of compounding pharmacies in the U.S. are accredited by the Pharmacy Compounding Accreditation Board (PCAB). That’s not a badge. It’s proof you do things right.
PCAB requires:
- 95% accuracy in dose verification tests
- Quarterly staff competency assessments
- Annual environmental monitoring reports
- Complete batch records for every preparation
Accredited pharmacies have 70% fewer errors than non-accredited ones. Dr. Robert Smith from Harvard found error rates in non-accredited pharmacies can hit 25%. That’s one in four prescriptions that could be wrong.
Yes, accreditation costs $15,000-$25,000 and takes over a year. But the cost of one lawsuit, one death, or one lost license? That’s priceless.
Use Technology - But Don’t Trust It Blindly
Software like Compounding.io and PharmScript can cut human errors by 40%. They flag dosage limits, check for drug interactions, auto-calculate concentrations, and generate electronic batch records.
But tech doesn’t replace judgment. One pharmacy in Texas relied on their software to verify a hormone cream formula. The formula was entered wrong. The software didn’t catch it because the input was flawed. Human error at the front end. Tech error at the back end.
Use AI tools like CompoundingGuard AI - they’ve reduced calculation errors by 87% in pilot programs. But always pair them with a second human check. Technology is your assistant, not your safety net.
Train Like Your Life Depends on It - Because It Does
Dr. Henry Cohen, former president of the International Academy of Compounding Pharmacists, says: ‘The single most effective error prevention strategy is quarterly competency assessments.’ Not annual. Quarterly.
Staff need 40+ hours of initial training on:
- Pharmaceutical math (calculation error rates must stay under 1%)
- Aseptic technique
- Equipment calibration
- USP standards
- Labeling requirements
Then, 8-12 hours of continuing education every year. Test them on real scenarios. Give them a prescription with a hidden error. See if they catch it.
And don’t forget the basics: handwashing, gowning, cleaning schedules. In one 2022 audit, 63% of non-accredited pharmacies had dirty hoods or expired disinfectants.
What Happens When You Skip These Steps?
Let’s be clear. Compounding isn’t just another pharmacy task. It’s high-risk, high-reward medicine. When done right, it gives a child a safe, flavored liquid for their seizure meds. It lets a cancer patient get chemo without the allergens in commercial formulations. It fills the gap when drugs are in short supply.
But when done wrong?
- A diabetic gets a compounded insulin with 10x the strength - and dies.
- An elderly patient gets a steroid injection contaminated with bacteria - and loses a limb.
- A parent gets a thyroid med with inconsistent dosing - and their child’s development is permanently affected.
The FDA reports that compounded medications make up just 1.5% of prescriptions - but 4.7% of medication error reports. That’s three times the risk. And it’s not because the science is hard. It’s because the process is rushed.
You can’t outsource safety. You can’t automate trust. You can’t cut corners and call it care.

CAROL MUTISO
December 18, 2025 AT 11:08