Heart failure isn’t a single disease-it’s a slow breakdown of the heart’s ability to pump blood. And while it sounds scary, the right medications can change the game. Four drug classes-ACE inhibitors, ARNI, beta blockers, and diuretics-are the backbone of modern treatment. They don’t cure heart failure, but they help you live longer, feel better, and avoid hospital trips. If you or someone you care about has been diagnosed with heart failure with reduced ejection fraction (HFrEF), understanding these four types of meds is essential.
ACE Inhibitors: The First Line for Decades
ACE inhibitors were the first heart failure meds proven to save lives. Captopril hit the market in 1981, and enalapril followed in 1985. They work by blocking the enzyme that turns angiotensin I into angiotensin II-a hormone that tightens blood vessels and makes the heart work harder. By stopping this, ACEIs lower blood pressure, reduce strain on the heart, and slow damage.
Common ones include enalapril, lisinopril, and ramipril. Starting doses are low-often just 2.5 mg once or twice a day-and slowly doubled every couple of weeks until you hit the target. For lisinopril, that’s 20-40 mg daily. The CONSENSUS trial in 1987 showed enalapril cut death risk by 27% in severe heart failure patients.
But they’re not perfect. About 1 in 5 people get a dry, annoying cough. It’s not an allergy-it’s a side effect from how the drug affects bradykinin in the lungs. Some people also see their potassium rise (hyperkalemia), especially if they have kidney issues. Rarely, swelling of the face or throat (angioedema) can happen. If that occurs, stop the drug immediately and get help.
ARNI: The New Gold Standard
For years, ACE inhibitors were the go-to. But in 2015, everything shifted with the approval of sacubitril/valsartan-better known as Entresto. This single pill combines two actions: it blocks angiotensin receptors (like an ARB) and inhibits neprilysin, an enzyme that breaks down helpful heart-protective hormones called natriuretic peptides. More of these peptides mean your body gets better at getting rid of salt and water, relaxing blood vessels, and reducing heart strain.
The PARADIGM-HF trial, which followed nearly 8,400 people across 47 countries, showed Entresto reduced the risk of death or hospitalization from heart failure by 20% compared to enalapril. That’s not a small win-it’s the biggest leap forward in heart failure treatment in decades.
Now, guidelines say ARNI should be the first choice for most people with HFrEF, replacing ACEIs outright. But there’s a catch: you can’t switch from an ACEI to ARNI unless you wait at least 36 hours. Do it sooner, and your risk of angioedema jumps by half a percent. That’s why doctors start ARNI at 24/26 mg twice daily and slowly increase to 97/103 mg twice daily over weeks.
Patients report real improvements. One Reddit user switched from lisinopril to Entresto and said their shortness of breath improved within two weeks. But others note more frequent urination at first. Cost is a barrier-Entresto runs about $550 a month without insurance, which is why adoption is slower in community clinics than in big hospitals.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards-how can slowing your heart help a weak heart? But beta blockers aren’t just for high blood pressure. In heart failure, they protect the heart from the harmful effects of stress hormones like adrenaline. Left unchecked, these hormones make the heart beat faster and harder, leading to more damage over time.
The three beta blockers proven to work in heart failure are carvedilol, metoprolol succinate, and bisoprolol. Carvedilol, for example, starts at 3.125 mg twice daily and is slowly doubled every two to four weeks. The COPERNICUS trial showed it cut death risk by 35% in severe cases. The CIBIS-II trial found bisoprolol reduced all-cause mortality by 34%.
Side effects are real. Fatigue, low blood pressure, and slow heart rate are common-especially when starting. Many patients feel wiped out at first. But here’s the thing: if you stick with it and titrate slowly, your heart gets stronger. One patient on Reddit saw their ejection fraction climb from 25% to 45% over 18 months. That’s not magic-it’s careful dosing and time.
Doctors won’t increase the dose unless your heart rate stays above 50 beats per minute and you’re not feeling dizzy or worse. If you’re tired, don’t quit. Talk to your provider. Sometimes a small tweak-like taking it at night-helps with fatigue.
Diuretics: Managing the Fluid, Not the Disease
Diuretics don’t improve survival. But they make life bearable. When the heart can’t pump well, fluid backs up into the lungs, legs, and belly. That’s when you feel swollen, winded, and heavy. Diuretics help you pee out the extra water.
Loop diuretics like furosemide, bumetanide, and torsemide are the go-to. Furosemide usually starts at 20-80 mg daily, adjusted based on how much you’re urinating. Torsemide might be better long-term-the EVEREST trial showed it led to 18% fewer hospitalizations than furosemide.
Thiazides like hydrochlorothiazide are used for milder cases or combined with loop diuretics. Spironolactone is a special case-it’s both a diuretic and a mineralocorticoid receptor antagonist (MRA). It blocks aldosterone, which causes salt and water retention. The RALES trial showed it cut death risk by 30% in advanced heart failure.
But diuretics come with trade-offs. Frequent bathroom trips can ruin sleep. Leg cramps are common because you’re losing potassium and magnesium. Many patients start taking supplements. One user on PatientsLikeMe said their cramps vanished after adding magnesium. But don’t self-prescribe-too much potassium can be dangerous, especially if you’re also on ACEIs or ARNIs.
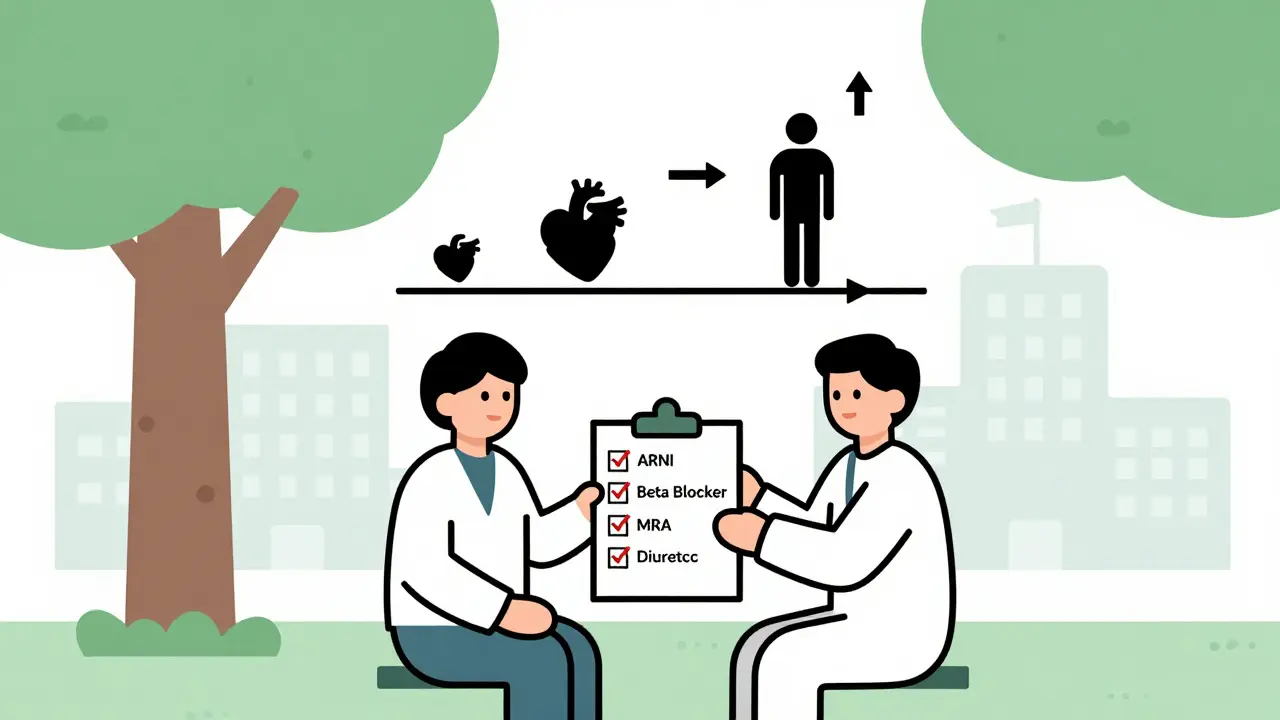
Putting It All Together: The Quadruple Therapy Approach
The best outcomes come from using all four classes together-but not all at once. The current standard is called quadruple therapy: ARNI (or ACEI/ARB if ARNI isn’t an option), beta blocker, MRA (like spironolactone), and SGLT2 inhibitor (like dapagliflozin). Diuretics are added as needed for symptoms.
Studies show this combo reduces death and hospitalizations by up to 21%. But here’s the problem: only 35% of eligible patients get all four meds within a year of diagnosis. Why? Titration is slow. Side effects scare people off. Costs block access. And many doctors still default to old habits.
Successful management needs a team. Heart failure clinics with nurses, pharmacists, and specialists get 85% adherence. General practices? Only 52%. If you’re not seeing a specialist, ask your doctor about a referral. Monitoring potassium, kidney function, and blood pressure is non-negotiable. You’ll need blood tests within 1-2 weeks of starting or changing any of these meds.
What If You Can’t Tolerate These Meds?
Not everyone can take ARNI or ACEIs. If you get a persistent cough from an ACEI, switching to an ARB like valsartan or losartan is a solid alternative. ARBs work similarly but don’t cause cough. The Val-HeFT trial showed valsartan reduced cardiovascular death by 33% in ACEI-intolerant patients.
If beta blockers cause too much fatigue, your doctor might lower the dose and extend the titration period. Some people do better on carvedilol than metoprolol-trial and error matters. For diuretics, switching from furosemide to torsemide can reduce side effects. And if cost is an issue, ask about patient assistance programs. Entresto has one, and many generic versions of ACEIs and beta blockers cost less than $10 a month.
Real Talk: What Patients Actually Experience
Online forums are full of honest stories. On Reddit, u/HeartWarrior2020 said furosemide gave them awful leg cramps until they started taking potassium and magnesium. u/PumpFailure switched from lisinopril to Entresto and noticed less breathlessness but more trips to the bathroom. u/CHFSurvivor said carvedilol slowly improved their ejection fraction-no miracle, just steady progress.
Amazon reviews tell a similar story. Diuretics get 4.1 out of 5 stars-people love the relief but hate the bathroom schedule. Beta blockers get 3.7-valued for long-term results, hated for the fatigue. ARNI gets 4.3-the highest rating-because people feel better, even if it’s expensive.
The bottom line? These meds work, but they’re not easy. Side effects are real. Titration is slow. But the payoff-living longer, breathing easier, staying out of the hospital-is worth it.
What’s Next?
Heart failure treatment keeps evolving. SGLT2 inhibitors (like dapagliflozin) are now recommended for all heart failure patients, even those with preserved ejection fraction. Vericiguat, a newer drug, adds another layer for high-risk patients. And ARNI’s approval is expanding-now it’s cleared for mildly reduced ejection fraction too.
But access remains uneven. In rural areas, only 28% of eligible patients get guideline-recommended therapy. If you’re in a small town or on a tight budget, advocate for yourself. Ask about generic options, financial aid, and telehealth follow-ups. You don’t need a fancy hospital to get good care-you just need the right information and persistence.
Can I stop my heart failure meds if I feel better?
No. Feeling better is a sign the meds are working, not that you no longer need them. Stopping ACEIs, ARNI, or beta blockers suddenly can cause your heart failure to worsen rapidly-even if you feel fine. Always talk to your doctor before making any changes.
Why do I need to take so many pills for heart failure?
Each medication targets a different part of what’s going wrong. ACEIs and ARNIs reduce strain on the heart, beta blockers protect it from stress hormones, MRAs block fluid-retaining hormones, and diuretics remove excess water. Together, they do more than any single drug alone. That’s why the combination cuts death risk by up to 20%.
Is ARNI better than ACE inhibitors?
Yes-for most people with HFrEF, ARNI is better. The PARADIGM-HF trial showed it reduces death and hospitalization more than enalapril. Guidelines now recommend ARNI as first-line therapy unless you can’t tolerate it. But if you’ve been stable on an ACEI for years, switching isn’t always necessary-talk to your doctor about your individual situation.
Can I drink alcohol while taking these medications?
Limit alcohol. It can lower blood pressure too much when combined with ACEIs, ARNIs, or beta blockers. It also weakens the heart muscle over time and can worsen heart failure. Most doctors recommend no more than one drink a day, if any. For some, complete abstinence is best.
How long does it take for these meds to start working?
Diuretics work fast-within hours or days, you’ll notice less swelling and easier breathing. But the life-saving effects of ACEIs, ARNI, and beta blockers take weeks to months. You won’t feel dramatically better right away, but studies show they reduce your risk of dying or being hospitalized over time. Stick with it-even if you don’t notice changes, your heart is being protected.
What should I do if I miss a dose?
If you miss a beta blocker or ARNI, take it as soon as you remember-if it’s not close to your next dose. If it’s almost time for the next one, skip the missed dose. Don’t double up. For diuretics, missing one dose won’t hurt, but don’t make a habit of it. Consistency matters most for the meds that save your life.
Next Steps: What to Do Now
If you’re on these meds, keep track of your symptoms, weight, and blood pressure. A sudden 2-3 pound weight gain in a day could mean fluid buildup. Write down side effects and bring them to your next appointment. Don’t wait until you’re struggling.
If you’re not on these meds but have been diagnosed with HFrEF, ask your doctor: ‘Am I on the full guideline-recommended therapy?’ If they say no, ask why. Is it cost? Side effects? Kidney function? There’s almost always a way forward.
Heart failure is a marathon, not a sprint. These medications are your best tools. They’re not perfect, but they’re proven. And with the right support, you can live well for years-even decades.
Jane Lucas
December 29, 2025 AT 01:56