More than 90% of prescriptions for older adults in the U.S. are filled with generic drugs. They’re cheaper, widely available, and approved by the FDA as equally effective as brand-name versions. But for people over 65, safety isn’t just about whether the active ingredient matches-it’s about how the body changes with age, how many pills are being taken, and whether the right drug is even being prescribed.
Why age changes how drugs work
Your body doesn’t process medicine the same way at 75 as it did at 45. As we age, our kidneys filter slower, our liver breaks down drugs less efficiently, and our body composition shifts-more fat, less water. That means a standard dose meant for a younger person can become an overdose for someone older.Studies show that by age 75, drug metabolism can drop by up to 30%. Take a common blood pressure pill like metoprolol. In a 60-year-old, it’s cleared from the body in about 4 hours. In an 80-year-old, it might stick around for 8 hours or longer. That extra time lets the drug build up, raising the risk of dizziness, slow heart rate, or even fainting.
Same goes for painkillers, sleep aids, and antidepressants. Older adults are more sensitive to the central nervous system effects of these drugs. A dose that helps a 50-year-old sleep might leave an 80-year-old confused, unsteady, or prone to falls. And falls in older adults aren’t just injuries-they can lead to fractures, hospital stays, and loss of independence.
Polypharmacy: The silent danger
The average Medicare beneficiary fills 48 prescriptions a year. Nearly 9 out of 10 are generics. But here’s the problem: the more pills you take, the higher the chance something goes wrong.Take two medications? Your risk of an adverse reaction is about 13%. Five medications? That jumps to 58%. Seven or more? It skyrockets to 82%. That’s not a typo. Eighty-two percent of older adults on seven or more drugs will experience some kind of negative reaction-drowsiness, nausea, confusion, bleeding, or worse.
Some drugs are especially risky when stacked together. Combining an opioid with a benzodiazepine (like Xanax or Valium) increases overdose risk by 154%. Mixing opioids with gabapentin (used for nerve pain) raises the chance of dangerous breathing problems by 70%. These aren’t rare cases. They’re predictable outcomes of poorly coordinated care.
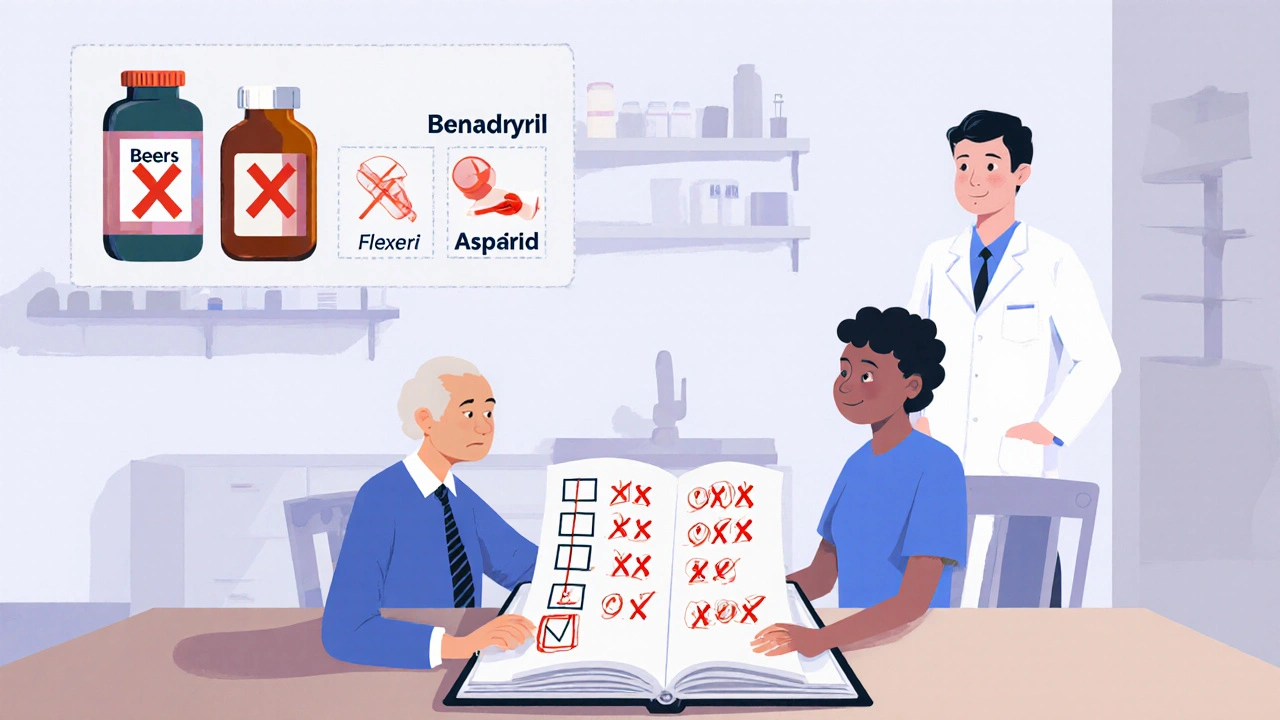
The Beers Criteria, updated in 2023 by the American Geriatrics Society, lists dozens of medications that should be avoided or used with extreme caution in older adults-no matter if they’re generic or brand-name. These include muscle relaxants like cyclobenzaprine (Flexeril), certain antihistamines like diphenhydramine (Benadryl), and even some antidepressants that increase fall risk by 37%.
Generic vs. brand: Is there a real difference?
The FDA says generic drugs must be bioequivalent to their brand-name counterparts. That means they deliver the same amount of active ingredient into the bloodstream within the same timeframe. For most drugs, this is true. But for some, small differences matter.Drugs with a narrow therapeutic index (NTI) are the big concern. These are medications where the difference between a safe dose and a toxic one is tiny. Warfarin (a blood thinner) is the classic example. Generic warfarin is 98.7% bioequivalent to brand-name Coumadin in clinical studies. But in real life, some older adults report unstable blood levels after switching. One study found 42% of seniors believe generic warfarin is less safe-even though there’s no proof it is.
Why the fear? Sometimes it’s the inactive ingredients. Generic pills might use different fillers, dyes, or coatings. For someone with a sensitive stomach or a swallowing problem, that change can cause nausea or make the pill harder to take. And when two generics look almost identical-say, two different brands of metformin-it’s easy to mix them up, especially with poor eyesight.
And then there’s perception. A 2022 Caregiver.org survey found 63% of family caregivers worried their elderly relatives’ generic meds weren’t working as well. In one case, an 82-year-old woman switched from brand-name Synthroid to generic levothyroxine and ended up with unstable thyroid levels, requiring three dose adjustments over six months. Her story isn’t unique. But it’s also not proof that generics are unsafe-it’s proof that switching meds in older adults needs careful monitoring.
What you can do to stay safe
The good news? Most generic drug risks aren’t about the pill itself-they’re about how it’s used. Here’s what actually helps:- Keep a full, updated list of every medication-including vitamins, supplements, and over-the-counter drugs. Bring it to every doctor visit. Duplicate prescriptions are a leading cause of adverse events.
- Ask for a medication review every 3-6 months if you’re on five or more drugs. Pharmacists can spot interactions, outdated prescriptions, and unnecessary pills. Studies show this cuts adverse events by 27%.
- Use a pill organizer. Color-coded containers or automated dispensers reduce errors by 34%. They’re especially helpful for people who take pills at different times of day or have memory issues.
- Check labels for large print. Sixty-five percent of adults over 65 have vision problems. If the label is too small, ask your pharmacist for a larger-font version or a printed list.
- Don’t assume a new pill is safe. Even if it’s a generic version of something you’ve taken before, ask: “Is this still right for me now?” Your needs change. So should your meds.
When to question a prescription
Some drugs just shouldn’t be given to older adults anymore. The Beers Criteria 2023 update made this clear:- Aspirin for primary prevention-no longer recommended for adults 70+ because bleeding risk outweighs any heart benefit.
- Direct oral anticoagulants (DOACs) like rivaroxaban-use with caution in those 75+ due to higher gastrointestinal bleeding risk.
- Sulfonylureas for diabetes-can cause dangerous low blood sugar, leading to falls and brain injury. Safer alternatives exist.
- Digoxin-still used, but only if closely monitored. Toxicity is common in older adults with kidney changes.
If your doctor prescribes one of these, ask: “Is this the safest option for someone my age?” There are often better, lower-risk alternatives.
It’s not about brand or generic-it’s about fit
The real issue isn’t whether your blood pressure pill is generic or brand-name. It’s whether it’s the right drug for your body right now. Older adults often have multiple chronic conditions-heart disease, diabetes, arthritis, depression. Most drug studies are done on healthy, younger people. That means prescriptions are often based on single-disease guidelines, not real-life complexity.As Dr. Michael Steinman from UCSF puts it: “The fundamental issue isn’t generic versus brand, but rather appropriate medication selection considering age-related changes and multimorbidity.”
Generic drugs saved Medicare billions. They make treatment accessible. But accessibility doesn’t mean safety by default. Safety comes from attention-careful prescribing, regular reviews, clear labeling, and open conversations with your pharmacist and doctor.
You don’t need to avoid generics. You just need to treat them like any other tool: use the right one, in the right way, for the right person.
Are generic drugs as safe as brand-name drugs for older adults?
Yes, for most medications, generic drugs are just as safe and effective as brand-name versions. The FDA requires them to deliver the same active ingredient in the same amount and at the same rate. But for older adults, safety depends less on whether a drug is generic and more on whether it’s appropriate for their age, kidney and liver function, and other medications they’re taking. Some drugs, like warfarin, require close monitoring after any switch-even between generics.
Why do some older adults feel generic drugs don’t work as well?
Some older adults report changes in how they feel after switching to a generic, especially with drugs like thyroid medication (levothyroxine) or blood thinners (warfarin). This isn’t always because the generic is less effective. It can be due to small differences in inactive ingredients, changes in pill size or shape affecting absorption, or even psychological concerns. In some cases, switching back and forth between generics can cause instability. That’s why it’s important to stick with one generic brand unless a doctor advises otherwise, and to get blood levels checked after any switch.
What medications should older adults avoid?
The 2023 Beers Criteria lists several medications to avoid or use with caution in adults 65+. These include: diphenhydramine (Benadryl), cyclobenzaprine (Flexeril), certain antipsychotics, benzodiazepines (like diazepam), and sulfonylureas (like glyburide). Even aspirin for heart protection is no longer routinely recommended for adults 70+. Always ask your doctor if a medication on your list is still necessary-or if a safer alternative exists.
How many medications are too many for an older adult?
There’s no magic number, but risk rises sharply after five medications. When someone is taking seven or more, the chance of a harmful reaction jumps to 82%. That’s why regular medication reviews are critical. A pharmacist can help identify duplicates, outdated prescriptions, or drugs that interact badly. The goal isn’t to take fewer pills-it’s to take the right ones.
Can I switch between different generic brands?
For most drugs, yes. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or some seizure medications-it’s best to stick with the same generic brand. Switching between different manufacturers can cause small changes in how the drug is absorbed, which can be dangerous. If you’re on one of these, ask your pharmacist to fill your prescription with the same generic each time. If that’s not possible, ask for blood tests to check levels after a switch.
What should I do if I think a generic drug is causing side effects?
Don’t stop taking it on your own. Write down the side effect, when it started, and how it affects you. Bring this info to your doctor or pharmacist. They can check if it’s a known reaction, if another medication could be causing it, or if switching back to the brand-name or a different generic helps. Sometimes it’s not the drug-it’s the dose. Older adults often need lower doses. A simple adjustment can fix the problem.

Katie Baker
November 15, 2025 AT 22:37