When you think about estradiol, you probably think about periods, mood swings, or menopause. But what you might not realize is that this hormone is also quietly running the show in your gut. Estradiol doesn’t just affect your reproductive system-it’s deeply involved in how your digestive tract works, how your gut bacteria behave, and even how sensitive your intestines are to pain and inflammation. If you’ve ever had bloating that seemed to follow your cycle, or noticed your IBS flares up right before your period, you’re not imagining it. There’s a real, measurable link between estradiol and your gut health.
What Estradiol Actually Does in Your Gut
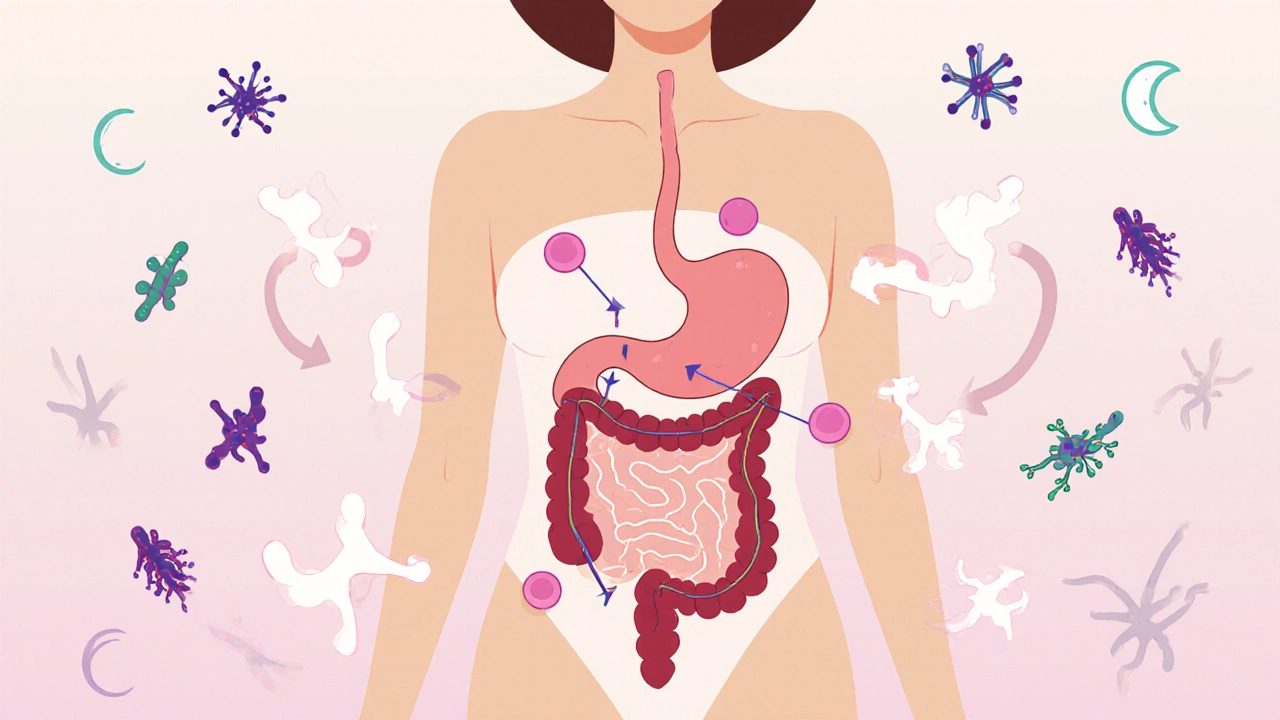
Estradiol is the most potent form of estrogen in your body. It’s made mostly in the ovaries, but fat tissue and even the gut itself can produce small amounts. And it doesn’t just float around waiting to affect your uterus. Estradiol receptors are found all over your gastrointestinal tract-from your stomach lining to your colon. That means your gut cells are literally wired to respond to this hormone.
When estradiol binds to these receptors, it triggers changes in gut motility. That’s the speed at which food moves through your digestive system. Too much estradiol? Your digestion can slow down, leading to constipation. Too little? You might get diarrhea. This is why so many women report digestive shifts during different phases of their cycle. Around ovulation, when estradiol peaks, many feel full faster or notice bloating. Right before their period, when estradiol drops, gut motility speeds up-and so does bowel movement frequency.
It’s not just about movement. Estradiol also helps maintain the tight junctions between the cells lining your intestines. These junctions act like gates, keeping bad bacteria and toxins from leaking into your bloodstream. When estradiol levels fall-like after menopause or during extreme stress-those gates can loosen. That’s called intestinal permeability, or "leaky gut." Studies have shown that postmenopausal women with low estradiol have higher markers of gut leakage than those on hormone therapy.
The Gut Microbiome and Estradiol: A Two-Way Street
Your gut bacteria don’t just sit there digesting food. They’re active players in hormone balance. One group of bacteria, called the estrobolome, specializes in metabolizing estrogen. These microbes produce an enzyme called beta-glucuronidase, which recycles estrogen back into your bloodstream instead of letting it be flushed out through stool.
Think of it like a recycling plant inside your gut. If your estrobolome is healthy and balanced, it keeps estradiol levels steady. But if your gut flora is out of whack-thanks to antibiotics, poor diet, or chronic stress-beta-glucuronidase levels can spike. That means too much estrogen gets recycled, leading to estrogen dominance. Or, if those good bacteria are missing, estrogen gets cleared too fast, causing low levels.
And it works the other way too. Estradiol shapes your microbiome. Higher estradiol levels are linked to more diverse gut bacteria, which is a sign of a healthy gut. In one 2023 study of women aged 35-55, those with naturally higher estradiol had 23% more microbial diversity than those with low levels. That diversity is linked to better digestion, lower inflammation, and even improved mood.

Why Hormonal Shifts Cause Digestive Trouble
Here’s the real-world impact: if you’re someone who struggles with IBS, constipation, or bloating, your hormones are likely playing a bigger role than you think. A 2022 review of 17 clinical studies found that over 70% of women with IBS reported symptom flare-ups tied to their menstrual cycle, especially in the days leading up to their period when estradiol drops.
It’s not just about irritation. Estradiol also affects your gut’s nervous system-the enteric nervous system, sometimes called your "second brain." Low estradiol can make your gut nerves more sensitive. That means normal gas or food movement feels painful. That’s why some women describe their IBS pain as "worse than cramps" during low-hormone phases.
And it’s not just cycles. Pregnancy, perimenopause, and even birth control pills can throw estradiol off balance. Women on combined oral contraceptives (which contain synthetic estrogen) often report less bloating and more regular bowel movements. On the flip side, women who stop hormonal birth control sometimes see a sudden spike in constipation or diarrhea as their natural hormone rhythm readjusts.
What You Can Do to Support Both Hormones and Gut Health
You can’t control your hormones entirely, but you can support your body’s ability to manage them. Here’s what actually works:
- Feed the estrobolome. Eat more fiber-rich foods like flaxseeds, lentils, oats, and cruciferous veggies (broccoli, kale, Brussels sprouts). Fiber feeds good bacteria and helps bind excess estrogen for elimination.
- Avoid sugar and processed fats. These feed bad bacteria that overproduce beta-glucuronidase, leading to estrogen buildup.
- Move regularly. Exercise helps clear excess estrogen through sweat and improves gut motility. Even 30 minutes of walking daily can make a difference.
- Manage stress. Cortisol-the stress hormone-directly interferes with estradiol production and gut barrier function. Try breathing exercises, yoga, or just 10 minutes of quiet time each day.
- Consider probiotics with Lactobacillus. Specific strains like Lactobacillus reuteri and Lactobacillus gasseri have been shown in clinical trials to help restore microbial balance and reduce bloating in women with hormonal digestive issues.
Some women find relief with magnesium supplements, which relax the gut muscles and ease constipation. Others benefit from DIM (diindolylmethane), a compound from cruciferous veggies that helps the liver process estrogen more efficiently. Always talk to a healthcare provider before starting supplements, especially if you’re on hormone therapy.

When to See a Doctor
If your digestive symptoms are new, worsening, or paired with other red flags-unexplained weight loss, blood in stool, severe pain, or irregular bleeding-it’s time to get checked. These could point to something like endometriosis, celiac disease, or inflammatory bowel disease, all of which can interact with hormonal changes.
But if your gut issues follow your cycle and improve after your period, you’re likely dealing with hormonally driven digestive sensitivity. In that case, working with a functional medicine practitioner or a women’s health specialist can help you map your symptoms to your cycle and tailor a plan that supports both your gut and your hormones.
It’s Not Just "All in Your Head"
For years, women with digestive issues tied to their cycle were told it was stress, anxiety, or "just PMS." But science now confirms: estradiol is a major player in gut function. Your gut isn’t broken. Your hormones are just out of sync with your lifestyle, diet, or life stage.
Understanding this link gives you power. You’re not stuck with bloating every month. You’re not doomed to IBS for life. You can take steps-dietary, lifestyle, and sometimes medical-to bring your hormones and your gut back into rhythm. It’s not about fixing your gut. It’s about supporting your whole system.
Does low estradiol cause constipation?
Yes. When estradiol levels drop-like after menopause or during the luteal phase of your cycle-gut motility slows down. This can lead to constipation, bloating, and a feeling of fullness. Estradiol helps keep the muscles in your intestines active. When it’s low, those muscles don’t contract as well, making it harder for stool to move through.
Can estradiol therapy help with IBS?
For some women, yes. Studies show that hormone replacement therapy (HRT) with estradiol can reduce IBS symptoms in postmenopausal women, especially bloating and abdominal pain. But it’s not a one-size-fits-all solution. Women with estrogen-sensitive conditions like certain types of breast cancer or blood clots may not be candidates. Always discuss risks and benefits with your doctor.
Does birth control affect gut health?
Yes. Combined birth control pills contain synthetic estrogen, which can stabilize hormone levels and reduce IBS flare-ups for some women. But others report increased bloating, yeast infections, or changes in bowel habits. The effect depends on the type of pill, your baseline gut health, and your body’s sensitivity to hormones.
Can gut bacteria affect estradiol levels?
Absolutely. The estrobolome-a group of gut bacteria-produces an enzyme that recycles estrogen back into your bloodstream. If your gut flora is imbalanced, this recycling can go too far (leading to high estrogen) or too little (leading to low estrogen). This is why fixing your gut can sometimes help balance your hormones, and vice versa.
What foods help balance estradiol and improve digestion?
Focus on fiber-rich plants: flaxseeds, chia seeds, broccoli, Brussels sprouts, lentils, and oats. These support good gut bacteria and help eliminate excess estrogen. Fermented foods like sauerkraut, kefir, and kimchi add beneficial bacteria. Avoid sugar, alcohol, and processed oils-they feed bad bacteria and worsen hormonal imbalance.
If you’ve been told your gut issues are "just stress" or "normal for women," remember: your hormones are real, your gut is listening, and you don’t have to live with constant discomfort. Small, consistent changes in diet and lifestyle can make a big difference-especially when you understand the connection between estradiol and digestion.
Akash Sharma
November 16, 2025 AT 02:42