For people with type 2 diabetes, the biggest threat isn’t high blood sugar-it’s the heart. About 65% of diabetes-related deaths are caused by heart disease. That’s not a coincidence. Diabetes doesn’t just affect your pancreas; it damages your blood vessels, raises blood pressure, and makes cholesterol behave badly. The good news? You don’t have to accept this fate. The most effective way to protect your heart isn’t just medication or just diet-it’s both, working together.
Why Diabetes and Heart Disease Are So Connected
When you have diabetes, your body struggles to manage glucose. That excess sugar in your blood doesn’t just sit there-it sticks to proteins in your arteries, making them stiff and inflamed. Over time, this leads to plaque buildup, narrowing the roads your blood flows through. High blood sugar also makes your blood more likely to clot, which can trigger a heart attack or stroke.
Most people with type 2 diabetes also have other risk factors: high blood pressure, excess weight, and abnormal cholesterol levels. These don’t happen by accident. They’re part of the same metabolic problem. The American College of Cardiology and American Heart Association have long recognized this link. In fact, since 2017, they’ve treated diabetes as a major cardiovascular risk factor-just like smoking or high cholesterol.
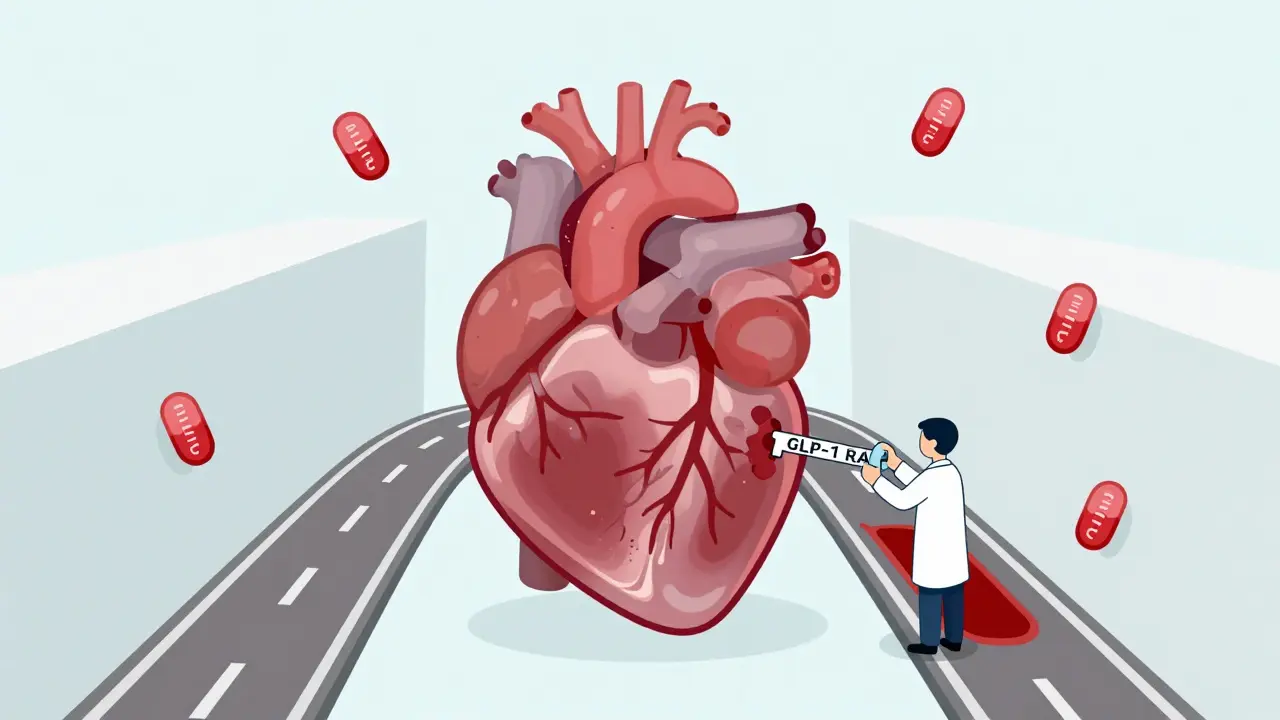
The New Generation of Diabetes Medications That Protect the Heart
For years, metformin was the go-to drug for diabetes. It helps with blood sugar and has some heart benefits. But newer medications do something metformin can’t: they directly lower your risk of heart attack, stroke, and death from heart disease.
GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro, Zepbound) are game-changers. These are injectable drugs that help your body release insulin only when needed, slow digestion, and reduce appetite. But their biggest win? They shrink your heart disease risk.
In the LEADER trial, liraglutide-a GLP-1 RA-cut major heart events by 13%. In the SELECT trial, semaglutide reduced heart attacks and strokes by 20% in people with obesity-even if they didn’t have diabetes. That’s why the FDA approved Wegovy in 2023 specifically for reducing cardiovascular risk in adults with heart disease and overweight or obesity. This wasn’t just another weight loss drug approval-it was a landmark shift.
And the numbers are striking. At the highest dose, semaglutide leads to an average weight loss of 14.9%. Tirzepatide? Up to 22.5%. That’s not just a few pounds. That’s enough to reverse metabolic damage and take pressure off your heart.
Lifestyle Changes That Actually Move the Needle
Medication alone isn’t enough. The real power comes from combining these drugs with proven lifestyle habits. The American Diabetes Association lays out clear, science-backed targets:
- Diet: Focus on Mediterranean, DASH, or plant-based patterns. No need to count carbs rigidly-just eat more vegetables, beans, whole grains, nuts, and fish. Cut back on processed foods, sugary drinks, and saturated fats.
- Exercise: At least 30 minutes a day, five days a week. You don’t need to run a marathon. Brisk walking, cycling, or swimming in 10-minute chunks counts. Studies show exercise reduces heart disease death risk by 27% in people recovering from cardiac events.
- Weight loss: Losing just 7% of your body weight cuts multiple heart risks-blood pressure, triglycerides, inflammation. The Look AHEAD trial proved this, though it didn’t fully stop heart events. That’s why combining it with medication is critical.
- Blood pressure: Keep it under 130/80 mm Hg. That’s stricter than the general public’s target because diabetes makes your vessels more vulnerable.
- Other habits: Don’t smoke. Limit alcohol. Sleep 7-8 hours. Manage stress. Stay socially connected. Each of these adds up.
Here’s the thing: lifestyle changes don’t just help your heart-they help your brain, your mood, and your energy. Medication can’t give you that.
The Synergy: Why Together They Work Better
One study of veterans with type 2 diabetes showed something powerful. Those taking a GLP-1 RA and following just four healthy habits saw a 40% lower risk of heart attack or stroke. But those who followed eight healthy habits-while on the medication-cut their risk by 63%.
That’s not additive. That’s multiplicative. The medication gives you the metabolic advantage-helping you lose weight, lower blood sugar, and reduce inflammation. Lifestyle fills in the gaps: it improves insulin sensitivity, lowers stress hormones, and strengthens your heart muscle through movement. It’s like giving your body a full tune-up instead of just fixing one part.
Even the FDA agrees. Their approval of Wegovy says it must be used “in addition to a reduced calorie diet and increased physical activity.” They didn’t just approve a pill-they approved a partnership between medicine and behavior.
A Paradigm Shift in Treatment
For decades, doctors told patients: “Try diet and exercise for six months first. If that doesn’t work, we’ll add medicine.” That’s outdated.
In June 2025, the American College of Cardiology released new guidance saying: “Patients should not be required to ‘try and fail’ lifestyle changes before starting medication.” Why? Because obesity is a chronic disease. Waiting delays care. And every month without control increases heart damage.
Now, doctors are encouraged to offer GLP-1 RAs as a first-line option for eligible patients-especially those with existing heart disease or high risk. That doesn’t mean lifestyle is less important. It means we stop treating it like a backup plan. It’s part of the core treatment.
And the numbers show why. Lifestyle alone typically leads to 3-5% weight loss. GLP-1 RAs deliver 10-22%. That’s the difference between modest improvement and dramatic change. But the most successful patients? They’re the ones who use the medication to make lifestyle changes stick.
What About Cost and Access?
Let’s be real: these drugs aren’t cheap. Semaglutide prescriptions rose by 317% between 2021 and 2023, but 40% of people who could benefit can’t get them because of insurance barriers. Some plans still require “failure” of cheaper drugs first-or won’t cover them for weight loss alone.
Still, the tide is turning. The $10 billion annual market projected for semaglutide by 2025 means manufacturers and insurers are under pressure to expand access. And as more evidence piles up-like the SELECT trial showing benefits even without diabetes-coverage is likely to improve.
If you’re struggling to get prescribed one, talk to your doctor about the cardiovascular benefits, not just weight loss. Cite the FDA approval and ACC guidelines. Ask for prior authorization with clinical evidence. Many patients succeed when they frame it as heart protection, not just weight management.
What’s Next?
Researchers are already looking at next-gen combinations-drugs that target both GLP-1 and GIP receptors, like tirzepatide, or even triple agonists in development. We’re moving toward personalized plans: using AI to match the right drug, dose, and lifestyle program to your body type, genetics, and habits.
By 2030, experts predict GLP-1 RAs will be standard for anyone with diabetes and heart risk. But the real win won’t be the drug. It’ll be the fact that people finally understand: your heart isn’t saved by a pill. It’s saved by the choices you make every day-with the help of the right tools.
Start today. Talk to your doctor about your heart risk-not just your blood sugar. Ask if a GLP-1 RA is right for you. And start with one lifestyle change: a 10-minute walk after dinner. Build from there. You’re not just managing diabetes. You’re protecting your heart.
Kayleigh Campbell
December 15, 2025 AT 04:00