LDAA Candidate Calculator
LDAA Eligibility Assessment
Determine if you or your patient qualifies for Low-Dose Azathioprine with Allopurinol therapy based on clinical criteria from the article.
When azathioprine doesn’t work-or makes you sicker-it’s not always the drug’s fault. Sometimes, it’s your body’s metabolism turning it into something harmful. That’s where azathioprine and allopurinol come in. This isn’t a random combo. It’s a carefully tuned medical strategy used by specialists to fix a hidden problem: toxic metabolite accumulation.
Why Azathioprine Can Backfire
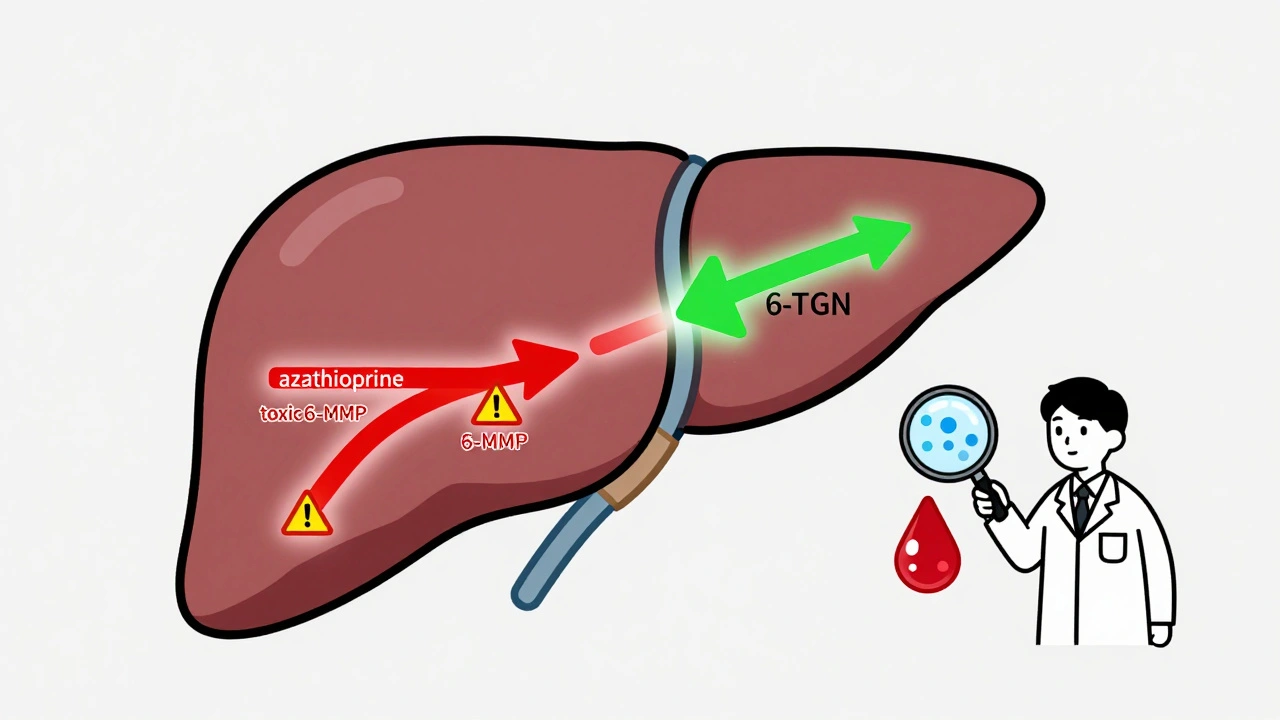
Azathioprine has been used for decades to treat autoimmune diseases like Crohn’s disease, ulcerative colitis, and autoimmune hepatitis. It works by calming the immune system. But here’s the catch: your body breaks it down into several different compounds. Two matter most. One is 6-thioguanine nucleotides (6-TGN). That’s the good stuff. It’s what actually suppresses inflammation. The other is 6-methylmercaptopurine (6-MMP). That’s the bad stuff. High levels of 6-MMP cause liver damage. And here’s the kicker: about 15-20% of patients naturally produce way too much 6-MMP. These are called ‘hypermethylators.’ Their bodies are just too good at making the wrong metabolite. If you’re one of them, you might be on azathioprine for months, feeling worse, with liver enzymes climbing-but your doctor can’t tell why. Standard tests don’t show the problem. You’re not allergic. You’re not noncompliant. You’re just metabolizing the drug the wrong way.How Allopurinol Changes the Game
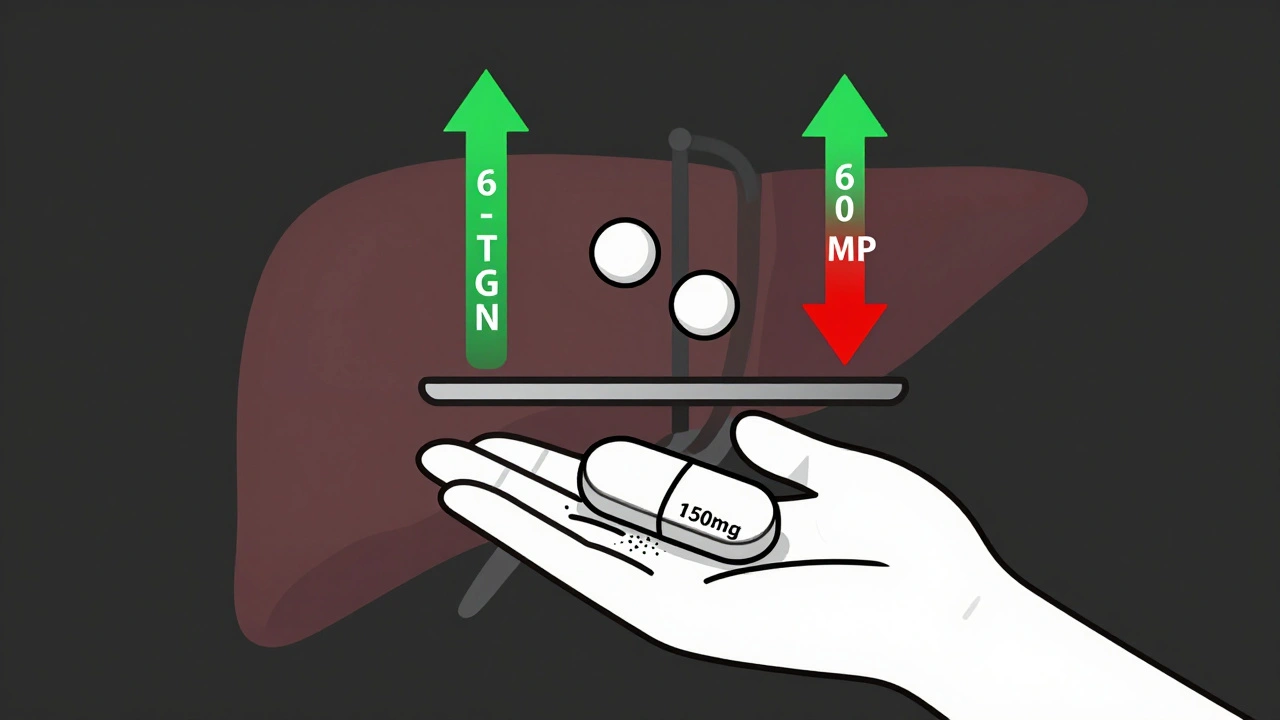
Allopurinol is usually prescribed for gout. It blocks an enzyme called xanthine oxidase. But that same enzyme also breaks down azathioprine’s intermediate form, 6-mercaptopurine (6-MP). When allopurinol shuts down xanthine oxidase, it forces the body to take a different path. Instead of turning 6-MP into toxic 6-MMP, your body redirects it toward 6-TGN. That’s the therapeutic metabolite. The result? A 70-90% drop in 6-MMP and a 2- to 5-fold rise in 6-TGN. In clinical studies, patients who couldn’t tolerate azathioprine alone saw their liver enzymes return to normal within weeks. This combo is called LDAA-Low-Dose Azathioprine with Allopurinol. It’s not about adding more drugs. It’s about using less azathioprine and letting allopurinol do the heavy lifting. The standard dose? Just 50 mg of azathioprine per day (down from 150-200 mg) and 100 mg of allopurinol.Who Benefits Most?
Not everyone. LDAA is targeted. It works best for people with high TPMT enzyme activity. TPMT is the enzyme that makes 6-MMP. If your TPMT level is above 14.2 U/mL, you’re likely a hypermethylator. That’s your sweet spot for LDAA. Patients with very low TPMT (under 5 U/mL) should avoid thiopurines altogether. Their bodies can’t handle even small doses-they’ll get severe bone marrow suppression. And if your kidneys are failing (creatinine clearance below 30 mL/min), allopurinol builds up and becomes dangerous. The best candidates are those who:- Have elevated liver enzymes on azathioprine
- Have high 6-MMP levels (>5,700 pmol/8×10⁸ RBCs)
- Have low 6-TGN levels (<230 pmol/8×10⁸ RBCs)
- Failed other treatments like anti-TNF drugs
The Risk: Myelosuppression
Here’s where things get serious. If you don’t reduce the azathioprine dose, LDAA can cause life-threatening bone marrow suppression. That means your white blood cell count crashes. You get fevers, infections, and sometimes sepsis. Early reports from the 1980s led to FDA warnings. But those were from patients who took full-dose azathioprine with allopurinol. Modern protocols fix that. The key is dose reduction. Studies show that with proper dosing (50 mg azathioprine + 100 mg allopurinol), the risk of severe neutropenia drops to under 10%. Without it? It’s 25-40%. That’s why monitoring is non-negotiable. Every patient starting LDAA needs:- Weekly complete blood counts for the first 4 weeks
- Therapeutic drug monitoring at 4 weeks to check 6-TGN and 6-MMP levels
- A 6-TGN target of 230-450 pmol/8×10⁸ RBCs
- A 6-MMP level below 2,800 pmol/8×10⁸ RBCs
Real Stories, Real Results
On patient forums, the feedback is split-but telling. One Reddit user, u/CrohnsWarrior2020, wrote: “After 3 years of failed Humira and azathioprine with sky-high liver enzymes, my GI put me on 50mg azathioprine + 100mg allopurinol. Liver enzymes normalized in 8 weeks. I’ve been in remission for 14 months.” Another, u/UlcerativeColitisNewbie, shared a different story: “Went on LDAA without proper monitoring. ANC dropped to 0.8. Hospitalized for 5 days with fever. Now terrified of all immunosuppressants.” The difference? Monitoring. The first patient had expert oversight. The second didn’t. A 2022 analysis of 37 patient reports found 86% had their liver toxicity resolved. But only when dosing and monitoring were done right.Why Isn’t Everyone Using It?
In Europe, 65% of IBD centers use LDAA routinely. In the U.S.? Only 35% of community clinics do. Why the gap? Many doctors learned to fear this combo because of old case reports. Others don’t have access to therapeutic drug monitoring. Blood tests for 6-TGN and 6-MMP aren’t available everywhere. And training is uneven. Fellowship programs report that it takes 3-6 months for new gastroenterologists to feel confident prescribing LDAA. That’s because it’s not just about the drugs. It’s about understanding metabolic pathways, interpreting lab values, and knowing when to pause. But the tide is turning. The American Gastroenterological Association updated its guidelines in 2023 to recommend LDAA as a preferred option for azathioprine-intolerant patients. The European Crohn’s and Colitis Organisation has endorsed it since 2020.Cost and Accessibility
Azathioprine costs about $20 a month. Allopurinol? $10. Together, LDAA therapy runs $1,200-$1,800 a year. Compare that to biologics like Humira or Stelara. Those cost $30,000-$50,000 a year. For patients without good insurance-or in countries with limited healthcare access-LDAA is a game-changer. It’s not just effective. It’s equitable.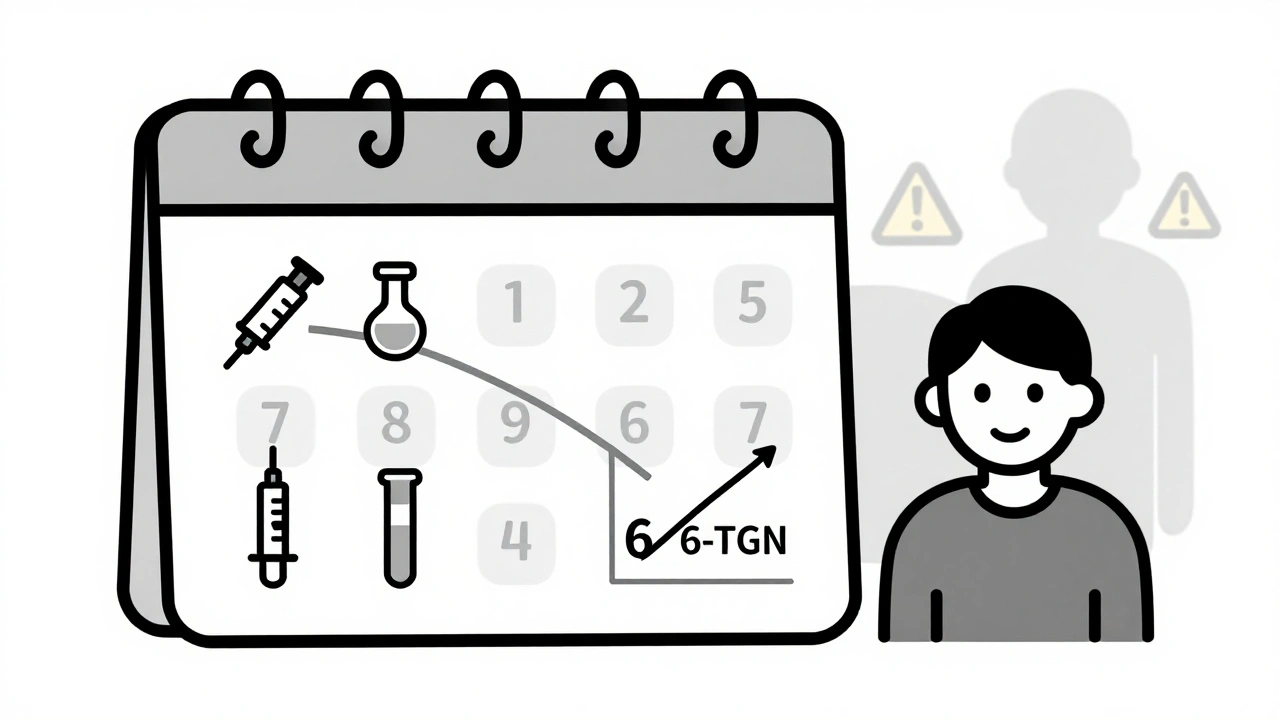
What’s Next?
Researchers are working on point-of-care tests that can measure 6-TGN and 6-MMP in minutes, not weeks. Two devices are in phase 3 trials. If they work, LDAA could become as routine as checking blood pressure. And it’s not just for IBD anymore. A 2023 study showed 82% of autoimmune hepatitis patients responded to LDAA after failing standard therapy. The future isn’t about replacing azathioprine. It’s about making it safer, smarter, and more personalized.Getting Started: The 4-Step Protocol
If you’re a patient and your doctor suggests LDAA, here’s what to expect:- Confirm you’re a candidate. You need high 6-MMP and low 6-TGN, or unexplained liver toxicity on azathioprine.
- Reduce azathioprine. Drop to 25-33% of your old dose. If you were on 150 mg, now you’re on 50 mg.
- Add allopurinol. 100 mg daily. No more, no less.
- Monitor like clockwork. Weekly blood counts for 4 weeks. Then every 2 weeks. At 4 weeks, get your 6-TGN and 6-MMP levels tested.
Final Thought
Azathioprine and allopurinol together aren’t a miracle cure. But for the right person, they’re a lifeline. They turn a drug that was making someone sick into one that brings remission. The science is solid. The evidence is strong. The risk? Manageable-if you know what you’re doing. This isn’t about using more drugs. It’s about using them better.Can azathioprine and allopurinol be taken together safely?
Yes-but only with strict dosing and monitoring. Combining full-dose azathioprine with allopurinol is dangerous and can cause fatal bone marrow suppression. When azathioprine is reduced to 25-33% of the standard dose (typically 50 mg/day) and allopurinol is given at 100 mg/day, the combination is safe and effective for patients with high 6-MMP levels. Weekly blood tests for the first month and therapeutic drug monitoring are essential.
What are the signs of toxic metabolite buildup from azathioprine?
The main signs are elevated liver enzymes (ALT, AST) without other causes like alcohol or viral hepatitis. Patients may feel fatigued, nauseous, or develop jaundice. In some cases, there are no symptoms until liver damage is advanced. Blood tests measuring 6-MMP levels above 5,700 pmol/8×10⁸ RBCs confirm hypermethylation, even if liver enzymes are borderline.
How long does it take for LDAA to work?
Liver enzymes usually normalize within 6-8 weeks. Clinical improvement in bowel symptoms may take 8-12 weeks. The key is not to stop too early. The full effect on 6-TGN levels and inflammation control often peaks around 12 weeks. Don’t assume it’s not working before then.
Do I need genetic testing before starting LDAA?
TPMT genetic testing is helpful but not required. The real test is metabolite levels: 6-MMP and 6-TGN in red blood cells. Someone with normal TPMT activity can still be a hypermethylator due to other factors. The gold standard is therapeutic drug monitoring-not genetics. TPMT testing is best used to rule out deficiency, not to confirm suitability for LDAA.
What happens if my white blood cell count drops on LDAA?
If your absolute neutrophil count drops below 1.5, pause azathioprine but keep allopurinol. Most patients recover fully within 1-2 weeks. Once counts normalize, restart azathioprine at 25 mg/day and increase slowly under monitoring. In 90% of cases, patients can return to full therapy without permanent damage. Never ignore a low count-it’s your body’s warning signal.
Is LDAA used outside of IBD?
Yes. In 2023, a study in Hepatology showed 82% of autoimmune hepatitis patients who failed standard azathioprine therapy achieved remission with LDAA. It’s also being studied in lupus nephritis and certain types of vasculitis. The mechanism-shifting metabolite balance-is relevant wherever thiopurines are used. But IBD remains the best-studied and most common application.
Can I take allopurinol without azathioprine?
Yes, but it won’t help your IBD. Allopurinol alone doesn’t treat inflammation. Its role in LDAA is purely metabolic-it redirects how azathioprine is processed. Taking it without azathioprine is only useful if you have gout or high uric acid. Never take allopurinol with azathioprine unless your doctor specifically prescribes the combo and monitors you.
olive ashley
December 5, 2025 AT 20:55