Alcohol & Diabetes Medication Safety Checker
Drinking alcohol while taking diabetes meds isn’t just a bad idea-it can be dangerous. For people managing diabetes with insulin, sulfonylureas, or metformin, alcohol doesn’t just add empty calories. It interferes with how your body controls blood sugar and how your liver works. And the risks aren’t always obvious. You might feel drunk, but what you’re really experiencing could be your blood sugar crashing. That’s not just uncomfortable-it can be life-threatening.
Why Alcohol Causes Low Blood Sugar
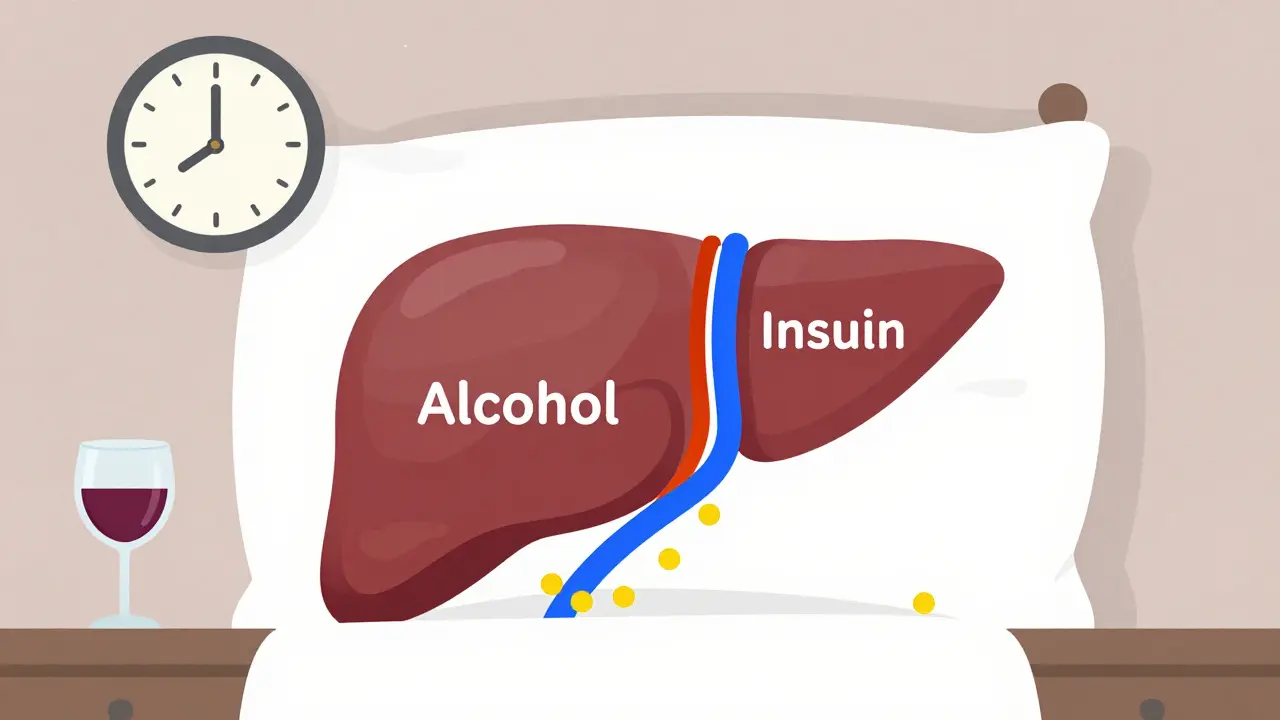
Your liver has two big jobs: detoxifying alcohol and keeping your blood sugar stable. When you drink, it drops everything to deal with the alcohol first. That means it stops releasing glucose into your bloodstream. If you’re on insulin or sulfonylureas like glipizide or glyburide, your body is already pushing to lower blood sugar. Add alcohol, and the system gets overloaded. Blood sugar can plunge-sometimes hours after your last drink. This isn’t just a quick drop. It can happen overnight. Many people with diabetes wake up confused, sweaty, or shaky because their blood sugar crashed while they slept. And here’s the scary part: the symptoms of low blood sugar-dizziness, slurred speech, confusion, weakness-look exactly like being drunk. If you pass out after a few drinks, someone might assume you’re just intoxicated. They might not check your blood sugar. They might not call for help. That’s how people end up in emergency rooms-or worse.Metformin and Alcohol: A Risky Mix
Metformin is one of the most common diabetes pills. It’s usually safe, but mixing it with alcohol ups the risk of something called lactic acidosis. This rare but serious condition happens when too much lactic acid builds up in your blood. Your liver normally clears it out, but when it’s busy processing alcohol, it can’t keep up. Symptoms include nausea, vomiting, stomach pain, muscle cramps, and extreme tiredness. If you feel this way after drinking, don’t wait-get medical help. Even without lactic acidosis, metformin and alcohol together can wreck your stomach. Both cause nausea, bloating, and diarrhea. When you combine them, those side effects don’t just add up-they multiply. One drink might be fine for some people. Two or three? That’s when things get messy. And if you’re already feeling sick from metformin, alcohol makes it worse.How Your Liver Gets Damaged
Your liver is the main filter for both alcohol and diabetes meds. When you drink regularly, especially heavily, your liver gets inflamed. Over time, that can turn into fatty liver disease, hepatitis, or even cirrhosis. These conditions make your liver less able to store and release glucose. That means your blood sugar becomes harder to control-no matter what meds you’re on. Alcohol also messes with the enzymes your liver uses to break down meds. The same enzymes that handle metformin, insulin, and other diabetes drugs also process alcohol. When alcohol floods the system, it slows down how fast your body clears the medication. That can make your meds work too hard-or too long-increasing the chance of low blood sugar. Even moderate drinking can cause this. You don’t have to be a heavy drinker for the risk to be real.
What Counts as a Safe Drink?
There’s no one-size-fits-all answer. The American Diabetes Association says it depends on your meds, your liver, your hypoglycemia awareness, and your overall health. But here’s what most experts agree on:- Never drink on an empty stomach. Always eat carbs with your drink-whole grains, fruit, or a small sandwich.
- Avoid sweet mixers. Soda, juice, and tonic water are full of sugar. Stick to seltzer, diet tonic, or water.
- Choose lower-sugar options: light beer, dry wine, or spirits with no added sugar.
- Limit yourself: one drink per day for women, two for men. That’s it.
- Check your blood sugar before you drink, during, and before bed. If it’s below 100 mg/dL, eat something first.
Why Timing Matters
Drinking at night is especially risky. Your liver is still working on alcohol while you sleep, and your body isn’t releasing glucose. If you took insulin or a sulfonylurea earlier in the day, the combo can cause a delayed drop. Many people don’t realize this until they wake up drenched in sweat, heart racing, or confused. Set an alarm. Check your blood sugar at 2 a.m. if you drank after dinner. Keep fast-acting glucose-glucose tabs, juice, or candy-right next to your bed. Tell someone you live with that you have diabetes. If you’re out, make sure a friend knows the signs of low blood sugar. Don’t assume they’ll know the difference between being drunk and being in danger.What About CGMs?
Continuous glucose monitors (CGMs) like the Dexcom G7 or FreeStyle Libre 3 are helpful. They show you real-time trends. If your glucose drops suddenly after drinking, you’ll see it. But here’s the catch: CGMs don’t detect alcohol. They only show your blood sugar. So if your number plummets, you still need to think: is this alcohol? That’s where your knowledge comes in. Use your CGM data to spot patterns. Do you always drop after two drinks? Then that’s your limit.
Connor Hale
January 3, 2026 AT 18:52