Alcohol Unit Calculator for Blood Thinners
Calculate Your Alcohol Units
One unit equals:
125ml wine (12% ABV), 3.6% beer (250ml), or 25ml spirits (40% ABV)
Binge Warning: More than 4 drinks in one sitting increases bleeding risk
What this means for you:
Important: Always inform your doctor about alcohol consumption. Even moderate drinking can affect your INR and bleeding risk.
If you’re on warfarin - the most common blood thinner still used today - you’ve probably heard mixed things about drinking alcohol. Some say it’s fine in moderation. Others warn it could land you in the hospital. The truth? It’s not about saying yes or no. It’s about understanding how alcohol changes your body’s response to warfarin, and what that means for your risk of bleeding.
How Warfarin Works - and Why INR Matters
Warfarin doesn’t thin your blood like water. It slows down clotting by blocking vitamin K, which your liver needs to make proteins that help blood clot. But it’s a tightrope walk. Too little, and you’re at risk for clots that can cause strokes or pulmonary embolisms. Too much, and even a minor bump can lead to dangerous bleeding. That’s where INR comes in. INR stands for International Normalized Ratio. It’s a standardized test that measures how long it takes your blood to clot. For someone not on blood thinners, a normal INR is between 0.8 and 1.1. If you’re on warfarin, your target range is usually 2.0 to 3.0 - sometimes up to 3.5 if you have a mechanical heart valve. Every 0.5-point rise above your target increases your bleeding risk by 30 to 50%.How Alcohol Throws Off Your INR
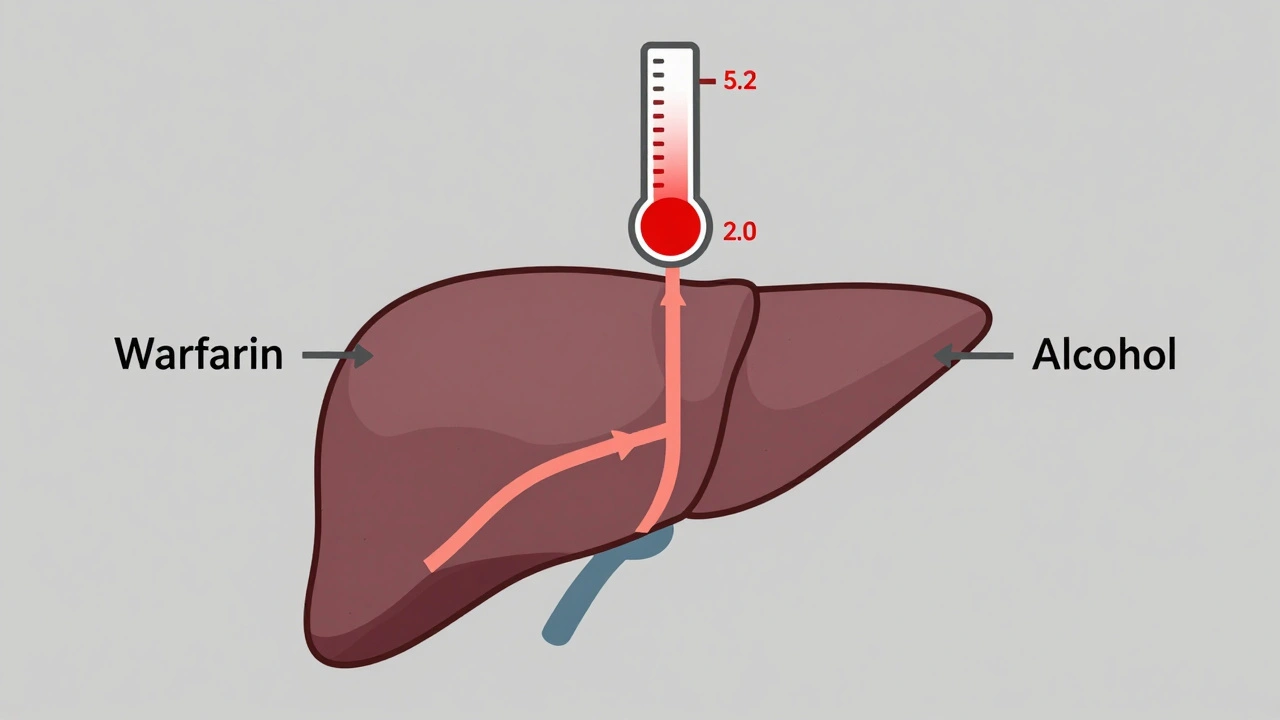
Alcohol doesn’t just make you feel loose - it messes with your liver’s ability to process warfarin. Your liver uses enzymes called CYP2C9 to break down warfarin. Alcohol competes for those same enzymes. When you drink, especially in large amounts, your liver gets overwhelmed. It can’t clear warfarin as quickly, so the drug builds up in your system. That pushes your INR higher, increasing bleeding risk. But it’s not that simple. Sometimes, heavy drinking over days or weeks can actually lower your INR. Why? Because chronic alcohol use damages your liver, reducing its ability to make clotting factors. That means your blood clots slower even without extra warfarin. So one week you might have a high INR, the next a low one - all because of alcohol. A 2012 study in the American Journal of Clinical Pathology found that among patients with INR levels above 9 - a dangerously high level - alcohol use was one of the top three reasons for bleeding complications, along with older age and kidney problems. In hospitalized patients with INR over 9, 35% had serious bleeding. About 17% died.Real Cases: When a Drink Turns Dangerous
Stories from patients aren’t rare. One 62-year-old man in New Zealand drank six pints of beer over two days while on warfarin. His INR jumped from 2.8 to 5.2 in 48 hours. He ended up with gastrointestinal bleeding and needed a hospital stay. On Reddit’s r/Warfarin forum, users share similar experiences. One person wrote: “I had four glasses of wine over the weekend. My INR went from 2.4 to 3.8. My doctor said this happens often.” Another said, “I thought one drink a night was fine - until I started bruising easily and had nosebleeds that wouldn’t stop.” These aren’t outliers. Research shows that 30 to 40% of people on warfarin drink alcohol regularly. For many, it’s not about binge drinking - it’s about consistency. A single glass of wine every night is less risky than saving all your drinks for Friday and going all out.Genetics Play a Bigger Role Than You Think
Not everyone reacts the same way to alcohol and warfarin. Your genes matter. Two specific gene variants - CYP2C9*2/*3 and VKORC1 1173G>A - affect how your body breaks down warfarin. People with these variants process the drug more slowly, meaning even small amounts of alcohol can cause big INR spikes. A 2015 NIH study found that patients with these genetic variants had a much higher risk of major bleeding when they drank alcohol, especially if they’d been on warfarin for over a year. The study showed a statistically significant interaction between alcohol use and these genes. In plain terms: if you have this genetic profile, your body is extra sensitive to alcohol’s effect on warfarin. Most doctors don’t routinely test for these variants - but if you’ve had unexplained INR swings or bleeding episodes, it’s worth asking.What’s Safe? The Numbers That Matter
There’s no magic number that says “this much alcohol is perfectly safe.” But there are clear guidelines based on evidence:- For men: No more than 14 units of alcohol per week, spread over at least three days. That’s about six standard drinks.
- For women: Same limit - 14 units per week.
- Never binge drink. That means more than four drinks in one sitting for men, or three for women.
- Avoid alcohol entirely if you’ve had a recent bleed, are sick, or are taking other medications that affect your liver.
What Counts as a Unit of Alcohol?
Knowing how much you’re drinking is half the battle. One unit equals:- Half a pint of normal-strength beer (3.6% ABV)
- A small glass of wine (125ml, 12% ABV)
- A single measure of spirits (25ml, 40% ABV)
Other Blood Thinners - Is Alcohol Still a Problem?
Warfarin isn’t the only option anymore. Newer drugs like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) are called DOACs - direct oral anticoagulants. They don’t require regular INR tests and have fewer food and drug interactions. But that doesn’t mean alcohol is safe with them. While DOACs don’t interact with alcohol the same way warfarin does, drinking heavily can still raise your bleeding risk. Alcohol irritates your stomach lining, increases blood pressure, and can cause falls - all of which raise the chance of internal bleeding. Plus, if you need emergency treatment for bleeding, DOACs don’t have easy reversal agents like vitamin K does for warfarin. If you’re on a DOAC, your doctor might say you can drink moderately. But they’ll still warn you: no binges. No daily heavy drinking. Stick to the limits.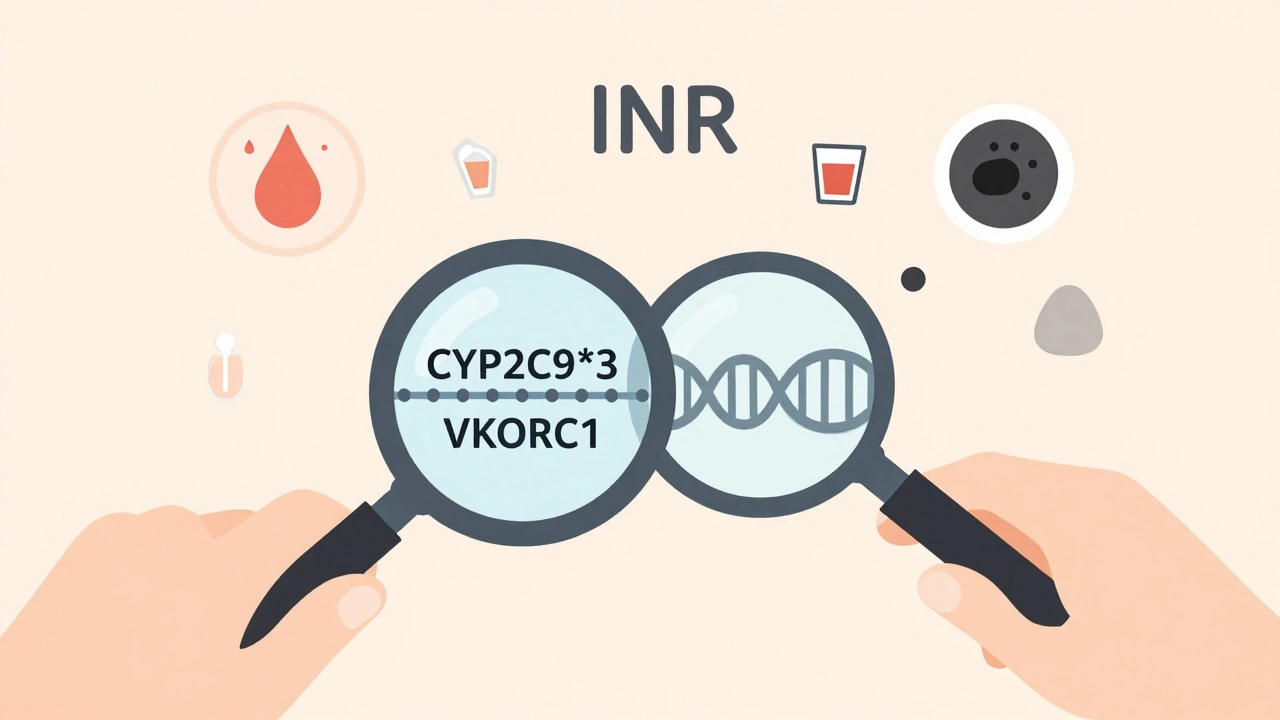
Warning Signs: When to Seek Help Immediately
If you’re on any blood thinner and drink alcohol, know the signs of dangerous bleeding:- Bleeding gums that won’t stop
- Nosebleeds lasting longer than 10 minutes
- Red or brown urine
- Black, tarry, or bright red stools
- Unusual bruising - especially without injury
- Heavier-than-normal menstrual bleeding
- Brown or bright red vomit - this could mean internal bleeding
- Sudden severe headache, dizziness, or confusion - could signal a brain bleed
What to Do If You Drink
If you choose to drink while on warfarin:- Keep it consistent. Don’t skip for weeks and then have a big night out.
- Never drink on an empty stomach. Food slows alcohol absorption.
- Stay hydrated. Alcohol dehydrates you, which can thicken your blood and make INR harder to predict.
- Let your doctor know if you’ve had more than usual - even if you think it’s no big deal.
- Get your INR checked more often after drinking - especially if you’ve had more than your usual amount.
The Bottom Line
You don’t have to give up alcohol completely if you’re on warfarin. But you do need to treat it like a medication - with rules, limits, and awareness. The goal isn’t perfection. It’s control. Consistent, small amounts are far safer than unpredictable binges. Your INR is a window into what’s happening inside your body. When alcohol enters the picture, that window gets foggy. The fewer times you fog it up, the clearer your picture stays. If you’re unsure - talk to your doctor. Bring your alcohol habits into the conversation. No judgment. Just facts. Because when it comes to bleeding risk, the smallest change can make the biggest difference.Can I have one glass of wine with warfarin?
Yes, one standard glass of wine (125ml) is generally safe if you drink it consistently and don’t exceed the weekly limit of 14 units. But even one drink can affect your INR if you’re genetically sensitive or have liver issues. Always tell your doctor if you drink regularly.
Does alcohol affect other blood thinners like Eliquis or Xarelto?
Alcohol doesn’t interact with DOACs like Eliquis or Xarelto the same way it does with warfarin - but heavy drinking still raises bleeding risk. Alcohol can irritate your stomach, increase blood pressure, and cause falls. It also makes it harder to reverse bleeding if it happens. Stick to moderate amounts and avoid binge drinking.
How long after drinking should I wait to get my INR checked?
If you’ve had more than your usual amount of alcohol, wait at least 48 hours before your next INR test. Alcohol can cause short-term spikes in INR, and testing too soon might show a false high reading. Always let your doctor know when you’ve been drinking so they can interpret your results correctly.
Why does my INR go up after I drink?
Alcohol slows down how fast your liver breaks down warfarin. This causes more warfarin to stay in your bloodstream, making your blood take longer to clot - which raises your INR. This effect is stronger if you drink heavily or binge drink. In some people, especially those with certain genes, even small amounts can cause big changes.
What should I do if my INR is too high after drinking?
If your INR is above 4.5 or you’re showing signs of bleeding, contact your doctor right away. They may advise you to skip your next warfarin dose, take vitamin K, or get plasma transfusion in severe cases. Never adjust your dose on your own. High INR with alcohol use is a medical red flag.
Is it safer to stop drinking entirely while on warfarin?
Stopping alcohol completely removes one variable from your INR equation - which can make your treatment more predictable. But for many people, moderate, consistent drinking is manageable with proper monitoring. The key isn’t always abstinence - it’s control. Talk to your doctor about what works best for your lifestyle and health history.
Colin Mitchell
December 3, 2025 AT 09:03